Discover the key factors that influence a woman’s fertility and learn about the optimal times for conception in this comprehensive guide.
When Is a Woman Most Fertile

Many women have wondered about the best time to conceive a child. Understanding female fertility is crucial for couples planning to start a family. It involves various factors, including hormones, the menstrual cycle, and identifying the fertile window.
The Role of Hormones in Female Fertility
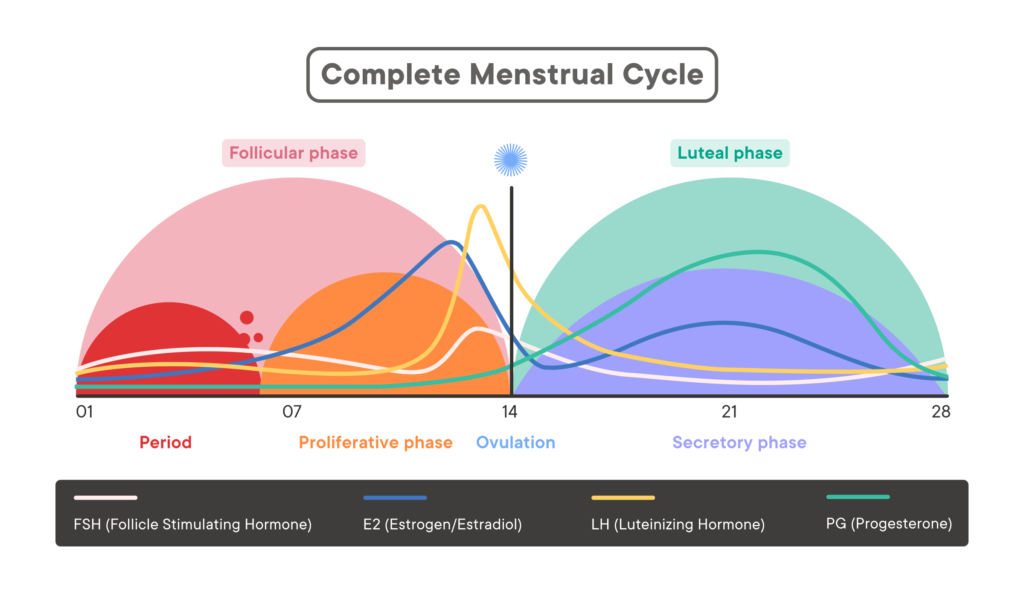
Hormones play a vital role in a woman’s fertility. The menstrual cycle is regulated by hormones, and specific hormones are responsible for ovulation. The follicle-stimulating hormone (FSH) helps stimulate the growth of eggs in the ovaries, while luteinizing hormone (LH) triggers ovulation.
During the menstrual cycle, estrogen levels rise, causing the uterine lining to thicken in preparation for a potential pregnancy. Progesterone levels increase after ovulation, supporting the uterine lining and sustaining a pregnancy. Hormonal imbalances can disrupt the fertility process, making it essential to maintain hormonal equilibrium.
The Menstrual Cycle and Fertility
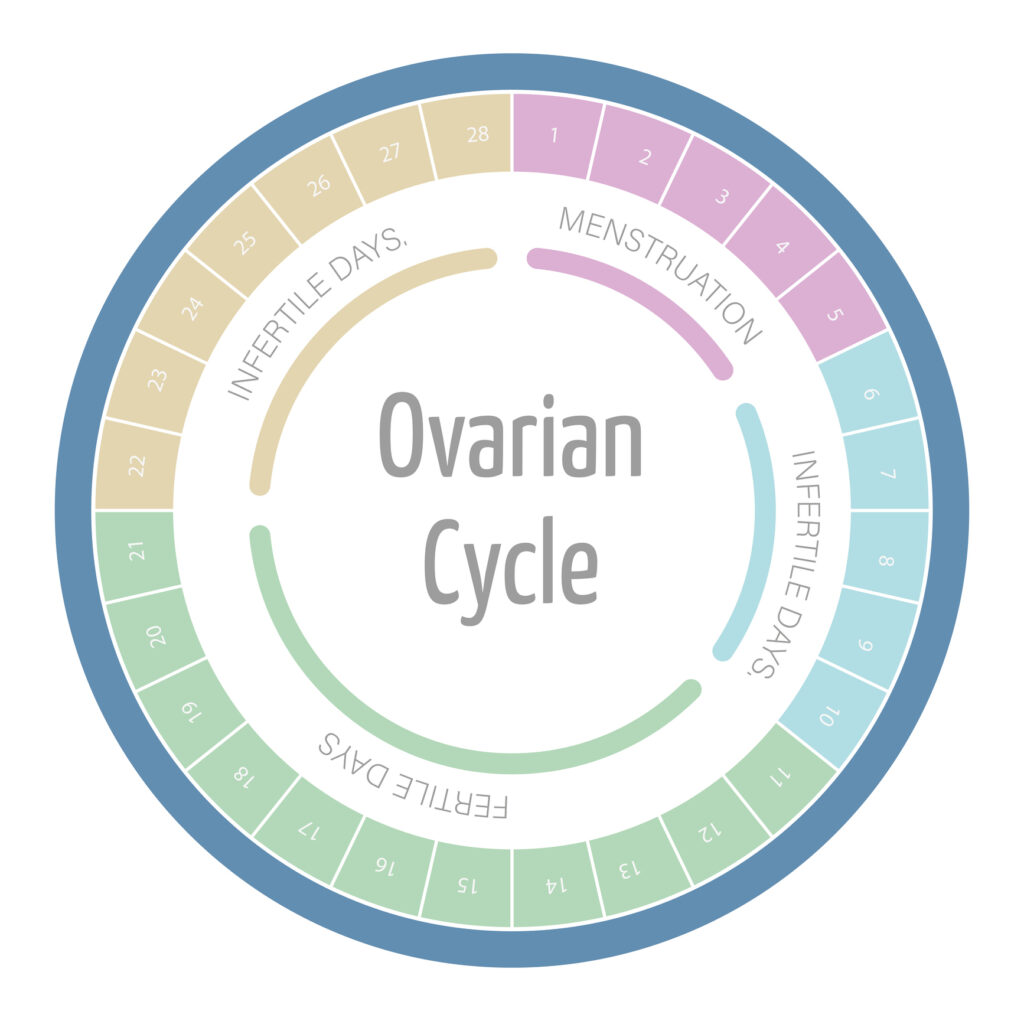
The menstrual cycle, typically lasting 28 to 35 days, consists of several phases. The follicular phase begins on the first day of menstruation and lasts until ovulation. During this time, follicles in the ovaries develop, and estrogen levels increase.
Ovulation occurs around the middle of the cycle when an egg is released from the ovary. This marks the start of the fertile window. The luteal phase follows ovulation and lasts until the next menstruation, during which the egg travels down the fallopian tube and the uterine lining thickens.
Now, let’s delve deeper into the fascinating world of female fertility. Did you know that the number of eggs a woman has is determined at birth? Yes, that’s right! Unlike men who produce new sperm cells throughout their lives, women are born with a finite number of eggs. This means that as a woman ages, her egg reserve gradually declines, leading to a decrease in fertility.
But don’t worry, it’s not all doom and gloom! While age does play a significant role in fertility, there are various factors that can influence a woman’s ability to conceive. Lifestyle choices, such as maintaining a healthy weight, avoiding excessive alcohol consumption, and not smoking, can positively impact fertility. Additionally, certain medical conditions, such as polycystic ovary syndrome (PCOS) or endometriosis, can affect a woman’s fertility and may require medical intervention.
Understanding your body and its unique fertility patterns can greatly increase your chances of conceiving. Charting your menstrual cycle, tracking basal body temperature, and monitoring cervical mucus changes are all methods that can help you identify your fertile window. By pinpointing the most fertile days in your cycle, you can optimize your chances of getting pregnant.
So, whether you’re just starting your journey to parenthood or have been trying for a while, remember that knowledge is power. Understanding the intricate workings of female fertility can empower you to make informed decisions and take proactive steps towards achieving your dream of starting a family.
Identifying the Fertile Window
Recognizing the fertile window is crucial for maximizing the chances of conception. The fertile window refers to the days when a woman is most likely to become pregnant. It typically lasts six days, including the day of ovulation and the five preceding it.
Understanding the intricacies of the menstrual cycle can provide valuable insights into fertility. The fertile window is influenced by various factors such as the lifespan of the egg, sperm, and the female reproductive system’s environment. By delving deeper into these biological processes, individuals can gain a better grasp of their fertility patterns.
Signs of Ovulation
Some women experience physical signs or symptoms that indicate ovulation. These can include mild pelvic pain, changes in cervical mucus consistency, or a small increase in basal body temperature. Monitoring these signs can help predict the fertile window.
Additionally, hormonal changes play a significant role in signaling ovulation. The surge in luteinizing hormone (LH) triggers the release of the egg from the ovary, marking the most fertile period of the menstrual cycle. Understanding the hormonal fluctuations that accompany ovulation can aid in pinpointing the fertile window with greater accuracy.
Tracking Menstrual Cycles
Tracking menstrual cycles is an effective way to identify the fertile window. By recording the start and end dates of each period, patterns can emerge. Online tools and mobile apps can help women track their cycles and predict ovulation more accurately.
Moreover, factors such as stress, diet, and lifestyle choices can impact the regularity of menstrual cycles. By maintaining a healthy lifestyle and addressing any underlying health issues, individuals can optimize their chances of conceiving during the fertile window. Taking a holistic approach to fertility tracking can provide a comprehensive view of reproductive health and enhance the understanding of the fertile window.
Factors Affecting Female Fertility
Several factors influence a woman’s fertility, including age and lifestyle choices. Understanding these factors is crucial for couples seeking to optimize their chances of conceiving.
Aside from age and lifestyle choices, there are other important factors that can affect female fertility. One such factor is underlying medical conditions like polycystic ovary syndrome (PCOS) or endometriosis, which can impact ovulation and the ability to conceive. Seeking medical advice and treatment for these conditions can help improve fertility outcomes for women facing such challenges.
Age and Fertility
Age plays a significant role in female fertility. Women are most fertile in their twenties and early thirties. Fertility gradually decreases in the late thirties and declines more rapidly after the age of 35. This is due to the depletion of ovarian reserve and the decrease in the quality of eggs over time.
While it is still possible to conceive in the late thirties and forties, the chances diminish significantly. It is important for women to be aware of their biological clock and consider starting a family earlier if possible.
Moreover, advancements in assisted reproductive technologies such as in vitro fertilization (IVF) have provided options for women facing age-related fertility challenges. These technologies can help women conceive later in life, although success rates may vary depending on individual circumstances.
Lifestyle Choices and Fertility
Lifestyle choices can also impact female fertility. Factors such as smoking, excessive alcohol consumption, and drug use can harm reproductive health. Maintaining a healthy weight and avoiding excessive stress can also positively affect fertility.

In addition to lifestyle choices, environmental factors such as exposure to toxins and pollutants can also influence female fertility. It is important for women to be mindful of their surroundings and take steps to minimize exposure to harmful substances that could potentially affect their reproductive health.
Fertility and Conception
Timing intercourse correctly is essential for maximizing the chances of conception. Knowing when a woman is most fertile can significantly improve the likelihood of getting pregnant.
Understanding the menstrual cycle and its various phases is crucial in determining the optimal time for conception. The fertile window, which typically spans a few days around ovulation, is when the chances of getting pregnant are highest. Ovulation predictor kits and tracking basal body temperature can help pinpoint this fertile window with greater accuracy.
Timing Intercourse for Optimal Fertility
Couples trying to conceive should aim to have intercourse during the fertile window. Having regular sexual intercourse every two to three days throughout the menstrual cycle can increase the chances of pregnancy.
It’s important to note that factors such as stress, age, and underlying health conditions can also impact fertility. Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can positively influence reproductive health and overall fertility.
Fertility Treatments and Interventions
In cases where natural conception does not occur, couples can explore fertility treatments and interventions. These include medications to stimulate ovulation, intrauterine insemination (IUI), and in vitro fertilization (IVF). Consulting a fertility specialist can help determine the most suitable treatment option for each couple.
Each fertility treatment option comes with its own set of considerations, success rates, and potential risks. It’s essential for couples to have a thorough understanding of these factors before proceeding with any fertility intervention. Emotional support and counseling are also crucial aspects of the fertility treatment journey, helping couples navigate the challenges and uncertainties that may arise.
Common Misconceptions About Female Fertility
There are various misconceptions floating around regarding female fertility. It is essential to distinguish between fact and fiction to make informed decisions regarding family planning.
Female fertility is a complex and intricate process influenced by various factors such as age, overall health, and genetics. Understanding the nuances of female reproductive health can help individuals make empowered choices when it comes to family planning.
Debunking Fertility Myths
One common myth is that a woman can only get pregnant on the day of ovulation. In reality, sperm can survive in the female reproductive tract for up to five days, meaning that pregnancy is possible even if intercourse occurs a few days before ovulation.
Moreover, fertility awareness methods, such as tracking basal body temperature and cervical mucus changes, can help individuals identify their most fertile days beyond just relying on ovulation predictors. By debunking these myths and understanding the intricacies of the female reproductive system, individuals can take proactive steps towards their fertility goals.
Understanding the Truth About Fertility
It is important to understand that fertility is not guaranteed, and each individual’s fertility journey is unique. While there are strategies to optimize fertility, factors beyond our control can affect the outcome. Seeking professional guidance and support can provide valuable insights and help navigate the complexities of fertility.
Furthermore, lifestyle factors such as diet, exercise, and stress management play a significant role in overall reproductive health. By adopting a holistic approach to fertility that encompasses both medical interventions and lifestyle modifications, individuals can enhance their chances of conceiving and maintaining a healthy pregnancy.