Learn about the intricate process of ovulation and find out when you are most fertile after your period.
When Do You Ovulate After Your Period?
Understanding the menstrual cycle is crucial for women who are trying to conceive. Ovulation, the release of an egg from the ovaries, plays a significant role in the fertility journey. But when exactly does ovulation occur after your period? Let’s explore the phases of the menstrual cycle, the process of ovulation, and how to track your ovulation effectively.
Understanding the Menstrual Cycle
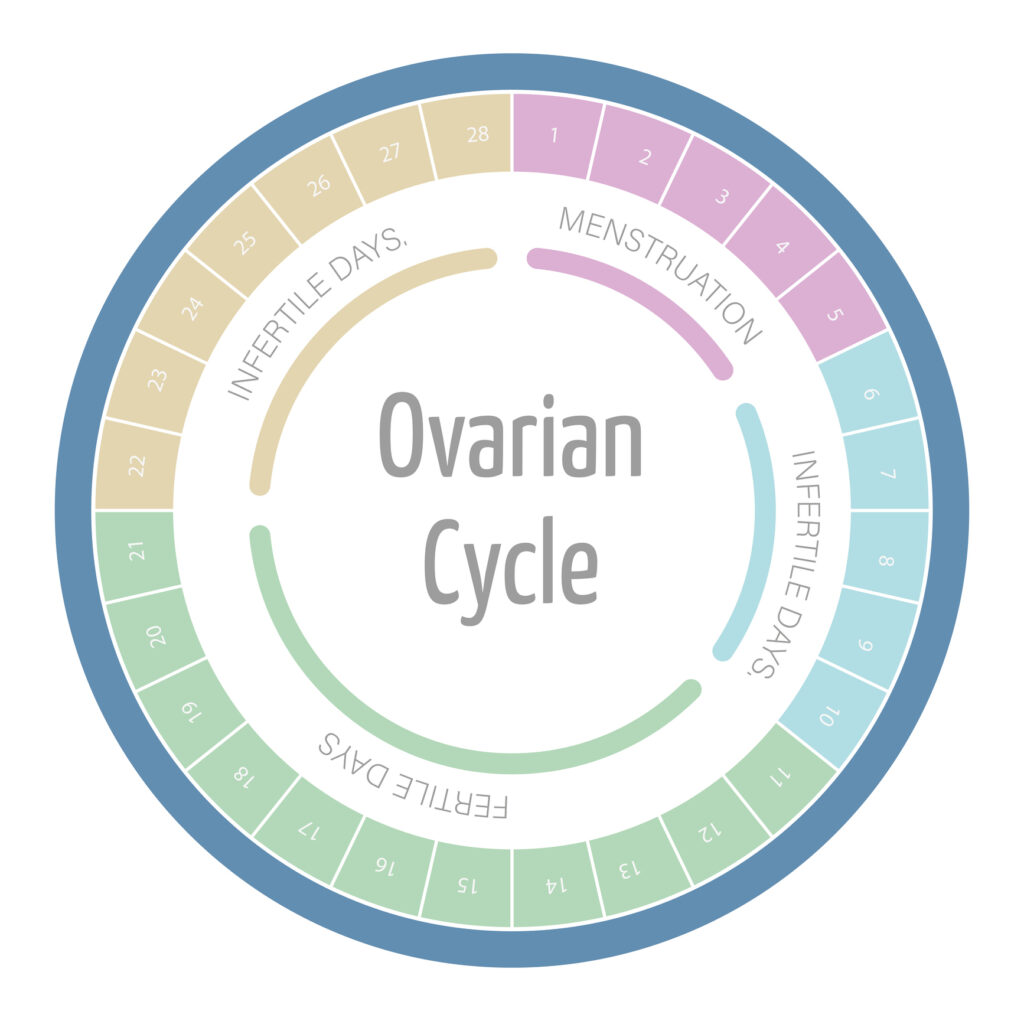
The menstrual cycle is a fascinating and intricate process that occurs in a woman’s body, preparing it for the possibility of pregnancy. While the average duration of the menstrual cycle is around 28 days, it’s important to note that this can vary from woman to woman. Understanding the different phases of the menstrual cycle is crucial in determining when ovulation occurs and the chances of conception.
The Phases of the Menstrual Cycle
The menstrual cycle consists of four main phases: menstruation, the follicular phase, ovulation, and the luteal phase. Each phase is unique and serves a specific purpose in the overall cycle.
Menstruation, also known as the period, is the first phase of the menstrual cycle. It involves the shedding of the uterine lining, which occurs when pregnancy does not take place. Typically lasting for about 3 to 7 days, menstruation is a natural process that marks the beginning of a new cycle.
Following menstruation, the follicular phase begins. This phase is characterized by the growth and development of follicles in the ovaries. These follicles contain immature eggs, and as the phase progresses, one follicle becomes dominant while the others regress. This dominant follicle continues to grow, preparing for the release of an egg.
Ovulation, the climax of the menstrual cycle, occurs after the follicular phase. It is a remarkable event where the mature egg is released from the ovary and is ready for fertilization. The egg then makes its way into the fallopian tube, where it awaits the presence of sperm for potential fertilization. If fertilization does not occur, the egg disintegrates, and the journey starts anew.
The luteal phase follows ovulation and lasts until the beginning of the next menstrual cycle. During this phase, the follicle that released the egg transforms into a glandular structure called the corpus luteum. The corpus luteum plays a vital role in preparing the uterus for potential implantation by producing progesterone. If conception does not occur, the corpus luteum degenerates, leading to the start of a new menstrual cycle.
Hormones and Their Role in the Menstrual Cycle
The menstrual cycle is intricately regulated by a delicate balance of hormones. These hormones work together to ensure the proper functioning of each phase and facilitate the chance of getting pregnant.
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) are two key hormones responsible for follicle development and ovulation. FSH stimulates the growth of follicles in the ovaries, while LH triggers the release of a mature egg from the dominant follicle.
Estrogen, another crucial hormone, plays a significant role during the follicular phase. As the follicles develop, estrogen levels rise, promoting the thickening of the uterine lining and increasing the production of cervical mucus. These changes create a favorable environment for potential fertilization and implantation.
During the luteal phase, progesterone takes center stage. The corpus luteum, formed from the follicle that released the egg, produces progesterone. This hormone prepares the uterus for potential pregnancy by further thickening the uterine lining and creating a nourishing environment for a fertilized egg. If pregnancy does not occur, the corpus luteum degenerates, leading to a decrease in progesterone levels and the start of a new menstrual cycle.
The menstrual cycle is a remarkable and complex process that occurs in a woman’s body. Understanding its phases and the role of hormones can provide valuable insights into fertility, reproductive health, and overall well-being.
The Process of Ovulation
Ovulation is an intricate and fascinating process that plays a crucial role in human reproduction. It involves a delicate interplay of various factors, including the ovaries, hormones, and precise timing. Understanding the complexities of ovulation can empower women with valuable knowledge to optimize their chances of conceiving.
During ovulation, the ovaries take center stage in the reproductive process. Within each ovary, multiple follicles are present, each containing an immature egg. These follicles undergo a dynamic process as the menstrual cycle progresses. One follicle emerges as the dominant one, continuing to grow and mature while the others disintegrate. The dominant follicle eventually reaches a critical point where it ruptures, releasing the fully developed egg into the fallopian tube.
As the released egg embarks on its journey through the fallopian tube, the window for fertilization opens. If sperm is present in the fallopian tube during this time, the egg may be fertilized, initiating the miraculous process of conception. Following fertilization, the newly formed embryo travels to the uterus, where it may implant itself in the uterine lining and develop into a pregnancy, marking the beginning of a new life.
The Lifespan of an Egg Post-Ovulation
Once the egg is released during ovulation, it has a relatively short lifespan of approximately 12 to 24 hours. For successful conception to take place, it is essential for sperm to be awaiting the egg’s arrival in the fallopian tube. Remarkably, sperm can survive within the female reproductive system for up to five days, underscoring the significance of timing intercourse strategically in the days leading up to ovulation. This prolonged sperm viability period enhances the likelihood of successful fertilization and underscores the importance of understanding the intricacies of the ovulation process.
Timing of Ovulation Post-Period
While the timing of ovulation can vary, there are general guidelines regarding the average timeframe for ovulation after menstruation.
Average Timeframe for Ovulation After Menstruation
In a typical 28-day menstrual cycle, ovulation usually occurs around day 14. This timing is based on an average cycle length and may not apply to everyone. Women with shorter cycles may ovulate earlier, while those with longer cycles may ovulate later.
Understanding the nuances of ovulation can be crucial for those trying to conceive or avoid pregnancy. Ovulation is a complex process influenced by various hormones, including estrogen and luteinizing hormone (LH). These hormones work together to trigger the release of an egg from the ovary, marking the most fertile period of a woman’s cycle.
It’s important to note that these calculations are approximate, and individual variations are common. Tracking your menstrual cycle patterns and using additional ovulation prediction methods can increase the accuracy of determining your ovulation window.
Factors Influencing Ovulation Timing
Several factors can influence the exact timing of ovulation in individual women. Stress, illness, travel, and hormonal imbalances can all affect the regularity and timing of ovulation. Additionally, certain medical conditions or medications may have an impact.
Women who are actively trying to conceive often rely on various methods to pinpoint their fertile window. From monitoring basal body temperature to observing changes in cervical position, these techniques can provide valuable insights into the timing of ovulation. Consulting with a healthcare provider or fertility specialist can also offer personalized guidance based on individual circumstances.
By understanding your body’s unique signs and symptoms of ovulation, you can gain insight into when you are most fertile. Tracking changes in your cervical mucus, body temperature, and using ovulation predictor kits can help pinpoint ovulation more accurately.
Signs and Symptoms of Ovulation
Ovulation is a crucial phase in a woman’s menstrual cycle, marked by a series of physical, emotional, and behavioral changes. Understanding and recognizing these signs can empower women to better understand their bodies and fertility.
During ovulation, the body undergoes various physical changes that can serve as indicators of fertility. One of the most notable physical signs is the increase in cervical mucus production, often described as resembling raw egg whites. This type of cervical mucus is considered fertile as it helps sperm survive and navigate more easily towards the uterus, increasing the chances of conception. Additionally, some women may experience mild pelvic pain or a sensation of twinging on one side of the lower abdomen, a phenomenon known as mittelschmerz, which can further signal ovulation.
Physical Signs of Ovulation
Increased cervical mucus that resembles raw egg whites is a common physical sign of ovulation. This fertile cervical mucus promotes sperm survival and allows easier passage into the uterus. Some women may also experience mild pelvic pain or a twinge on one side of the lower abdomen, known as mittelschmerz.
Emotional and behavioral changes are also prevalent during ovulation, affecting a woman’s mood and overall demeanor. It is not uncommon for women to notice heightened sexual desire and an increased sense of energy and well-being during their fertile window. These emotional fluctuations are closely tied to hormonal shifts that occur throughout the menstrual cycle, influencing a woman’s perception and behavior.
Emotional and Behavioral Changes During Ovulation
Ovulation can also impact a woman’s mood and behavior. Some women may notice heightened sexual desire and a general feeling of increased energy and well-being during their fertile period. These changes are influenced by hormonal fluctuations throughout the menstrual cycle.
Tracking Your Ovulation
Tracking your ovulation can significantly increase your chances of conceiving. Several tools and methods can help you determine your most fertile days.
Understanding your menstrual cycle is key to tracking ovulation. The menstrual cycle is divided into two main phases: the follicular phase and the luteal phase. Ovulation typically occurs around the middle of the cycle, approximately 14 days before your period starts. By pinpointing this timeframe, you can identify when you are most likely to conceive.
Ovulation Prediction Kits
Ovulation prediction kits detect the surge of luteinizing hormone (LH) in your urine, which occurs approximately one to two days before ovulation. These kits are readily available over-the-counter and can provide valuable information about your fertility window.
It’s important to note that ovulation prediction kits may not be foolproof for every woman. Factors such as irregular cycles or certain medications can affect the accuracy of these kits. Therefore, combining multiple tracking methods can offer a more comprehensive view of your ovulation patterns.
Fertility Charting and Natural Methods
Charting your basal body temperature and monitoring changes in your cervical mucus throughout your cycle can also help predict ovulation. Fertility awareness methods, such as the sympto-thermal method, combine these indicators to determine your fertility status accurately.
Additionally, paying attention to other signs of ovulation, such as changes in libido, breast tenderness, and abdominal discomfort, can further enhance your understanding of your cycle. These subtle cues, when combined with other tracking methods, can provide a more holistic approach to predicting ovulation.
In conclusion, understanding when you ovulate after your period is crucial when trying to conceive. By familiarizing yourself with the phases of the menstrual cycle, tracking physical and emotional signs, and utilizing ovulation prediction methods, you can optimize your chances of achieving pregnancy. Remember, every woman’s body is unique, and it’s essential to listen to your body’s signals and consult a healthcare professional for personalized guidance.