Uncover all the information you need about getting pregnant at a late age
The relevance of age
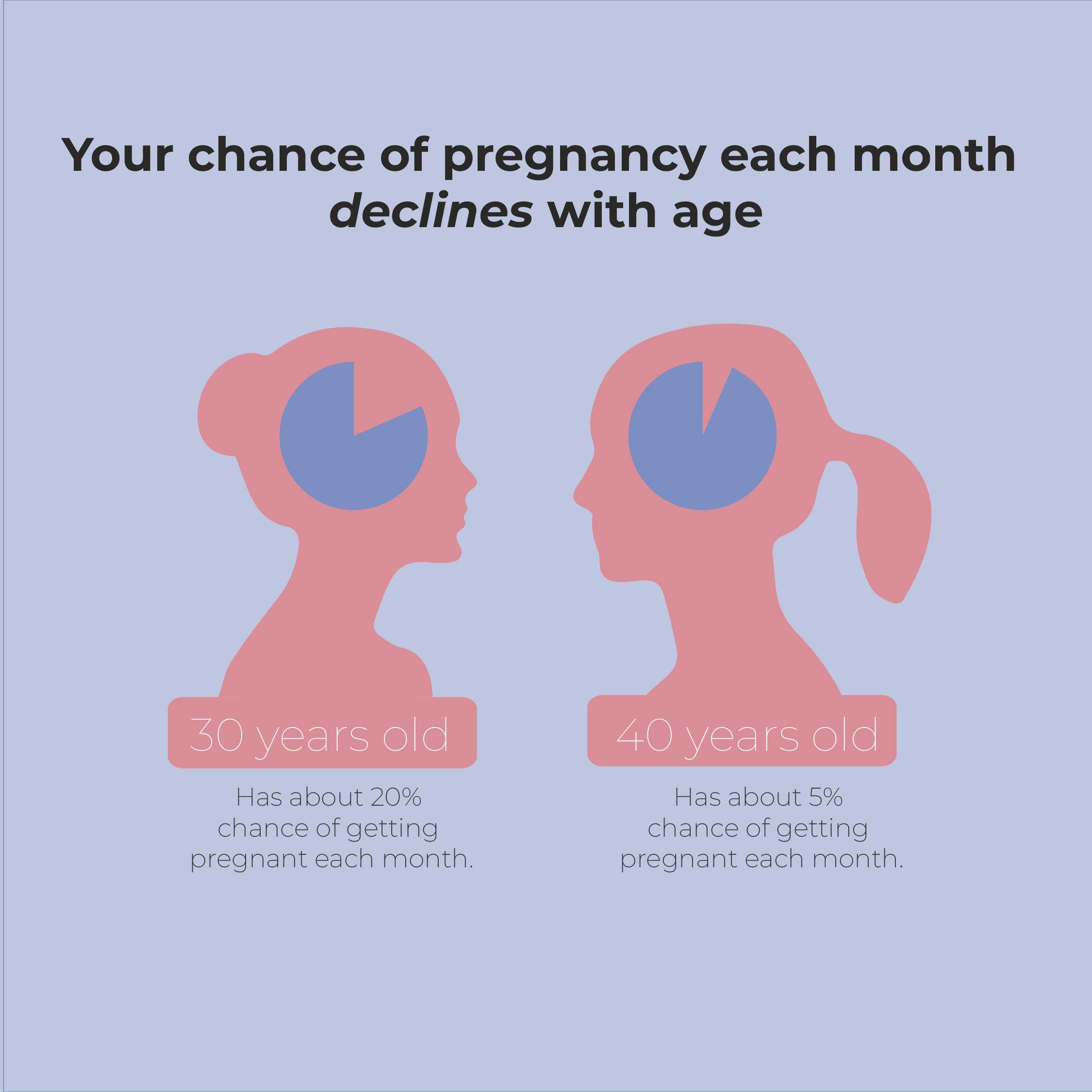
According to research over the last 40 years, a healthy 30 year old woman has about a 20% chance of getting pregnant each month. A healthy, ovulatory 40-year-old woman’s chance per month is 5% (1,6). The decline is slow and steady up until the age of about 35. After that the decline becomes steeper. These ranges and time frames have been established through multiple studies and have been consistent for the last 30+ years. Getting pregnant after 40 the decline in fertility is attributed to depletion of ovarian oocyte (eggs) reserve and is determined by genetic, environmental, and lifestyle factors.(2).

What makes it hard to get pregnant after 35 or 40?
Although your changes of getting pregnant after 35 or 40 are decreasing, there are good news. Age at conception does have bearing on time to pregnancy in a healthy, ovulatory woman. In general, fecundity (a woman’s physiological ability to have a child) is reported as age ranges because it is difficult to correlate a specific age to a specific chance of success. There are also factors that can affect reproductive aging. These include other medical conditions that can have an effect such as endometriosis, fibroids, genetic conditions (errors in number of chromosomes), environmental influences, obesity, smoking, thyroid gland dysfunction, history of sexually transmitted diseases (STDs), and ovulatory dysfunction, to name a few (2,3).
PCOS stands for Polycystic Ovarian Syndrome, it is the most common form of ovulatory ovarian dysfunction. The pathology of PCOS makes ovulation irregular and unpredictable, making the timing of intercourse for conception difficult and mostly trying to get pregnant after 40.
There could also be issues with male fertility such as erectile dysfunction and sperm quality issues. Male evaluation initially consists of a semen analysis and potentially other endocrine blood testing to evaluate any severe sperm abnormality.
How can fertility specialist can help to conceive after 35 or 40?
Most of the factors other than extreme reproductive age are usually treatable. When you start you journey to get pregnant after 40, the first step is a comprehensive evaluation of both you and your partner (if applicable). We test your ovarian reserve to gauge likelihood of adequate number of eggs produced per cycle, prolactin levels since the elevated levels can affect regularity of ovulation, and PCOS testing. If there are any positive findings, we can offer prescription medications or supplements beneficial for conception (5).
There are supplements that both partners can take that have been shown to be beneficial for conception and getting pregnant after 40. Lifestyle modification and diet changes (such as following the Mediterranean diet) can also positively impact your chances to get pregnant after 40. Controlling your stress and regular moderate exercise also confer benefits (3,4).
The journey
Getting pregnant after 40 years old, especially in the face of infertility challenges, is a complex and emotional journey that many individuals and couples find themselves navigating. The desire for parenthood does not diminish with age, and the longing to conceive and welcome a child into one’s life remains strong. While fertility may decline with age, it’s essential to acknowledge that getting pregnant after 40 is not impossible, and there are various avenues to explore on this remarkable path.
In the midst of infertility concerns, it is crucial to seek expert guidance and remain informed about the available options. Fertility treatments, such as in vitro fertilization (IVF) and the use of donor eggs, have proven to be successful for many individuals in their 40s, offering renewed hope and possibilities. Additionally, maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can positively impact fertility, no matter one’s age.
Moreover, the relevance of emotional support cannot be overstated. The emotional toll of facing infertility and the challenges of getting pregnant after 40 can be overwhelming. Finding a support network, whether through friends, family, or support groups, is crucial in navigating the ups and downs of this journey.
Conclusion
In conclusion, while getting pregnant after 40 may present unique challenges, it is a goal within reach for many. Infertility should not be a deterrent, but rather a call to explore the many available options and seek professional advice. With perseverance, emotional support, and the right approach, individuals can overcome obstacles and realize their dreams of parenthood even at an age when conventional wisdom might suggest otherwise.
Please click the link below for a consultation with an experienced Reproductive Endocrinologist. You can also follow us on Facebook or return to our website for updated information about your fertility journey.