Discover why your cycles may not return for months or a year after stopping birth control.
Understanding Post-Birth Control Syndrome
Many individuals who discontinue hormonal birth control methods, such as the pill, patch, ring, or hormonal IUD, expect their menstrual cycles to resume immediately or within a few weeks. However, for some, the return of regular cycles can be delayed for several months or even up to a year. This phenomenon is often referred to as post-birth control syndrome (PBCS), although it is not formally recognized as a medical diagnosis.
Post-birth control syndrome describes a range of symptoms and menstrual irregularities that occur after stopping hormonal contraception. These symptoms can include irregular or absent periods, mood changes, acne, and other hormonal imbalances. Understanding the underlying hormonal regulation and recovery process is essential to grasp why cycles may not return promptly.
Hormonal Regulation and Recovery
Hormonal birth control works primarily by suppressing the natural hormonal cycle to prevent ovulation. Synthetic hormones like estrogen and progestin provide steady hormone levels that trick the body into thinking it is already pregnant, thereby halting the release of eggs from the ovaries. When birth control is discontinued, the body must readjust and restart its own hormonal rhythm.
This adjustment period can vary widely depending on individual factors. The hypothalamic-pituitary-ovarian (HPO) axis, which regulates the menstrual cycle, may take time to resume normal function. In some cases, the suppression caused by hormonal contraception can lead to a temporary imbalance or delay in the secretion of gonadotropin-releasing hormone (GnRH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH), all critical for ovulation and menstruation.
It’s important to note that while many people experience a quick return to fertility and regular cycles, others may face a longer recovery period. According to the Centers for Disease Control and Prevention (CDC), fertility generally returns quickly after stopping birth control, but individual experiences can differ significantly. Factors such as age, overall health, and the duration of birth control use can all play a role in how quickly one’s body readjusts to its natural hormonal state.
Common Timeline for Menstrual Return
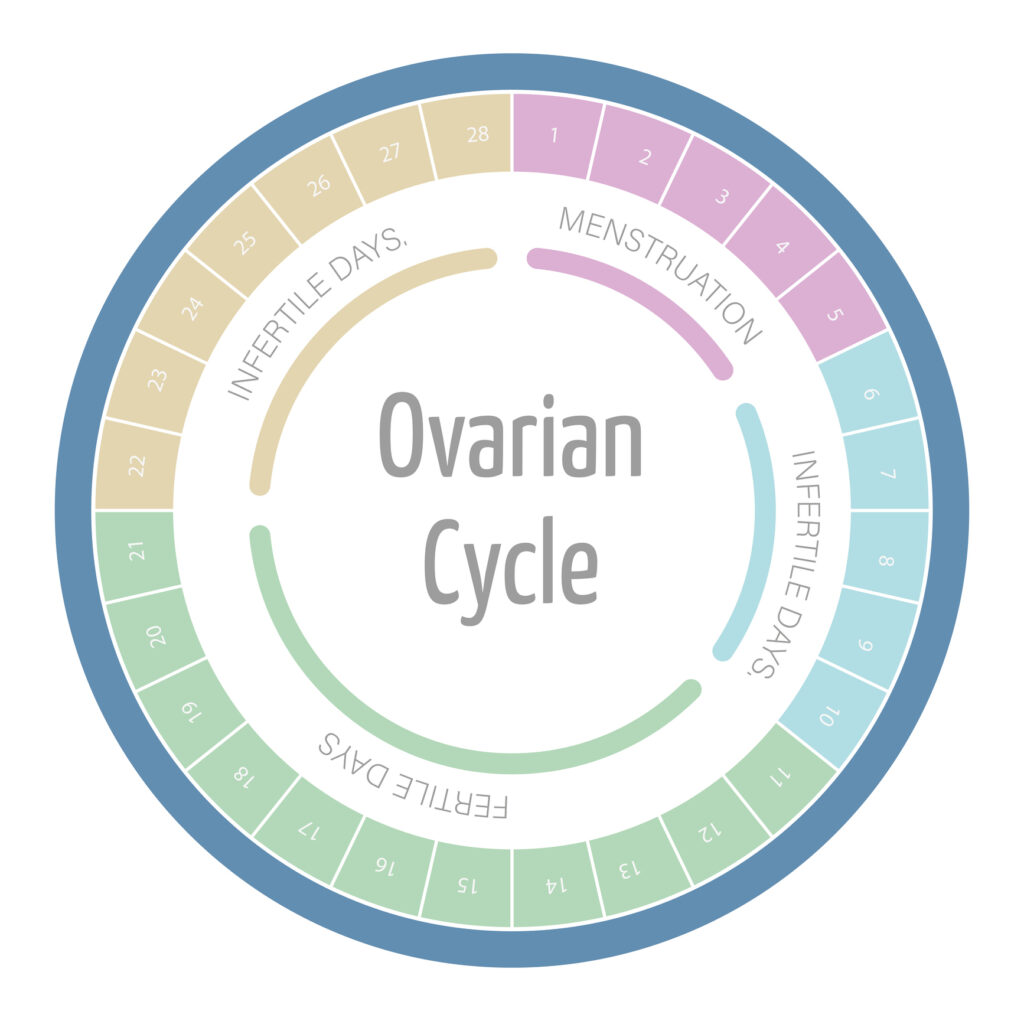
For most individuals, menstrual cycles return within one to three months after stopping hormonal contraception. Ovulation usually resumes within this timeframe, allowing for the possibility of pregnancy. However, delays beyond three months are not uncommon and can be influenced by the type of birth control used and individual health factors.
For example, the contraceptive injection (Depo-Provera) is known to cause longer delays in menstrual return, sometimes taking up to a year for cycles to normalize. In contrast, oral contraceptive pills typically allow for quicker resumption of cycles once discontinued. The variability in timelines can be confusing and frustrating for those eager to conceive or simply regain hormonal balance.
It’s also important to recognize that the first few cycles after stopping birth control may be irregular or different in flow and duration compared to pre-contraceptive cycles. This irregularity is part of the body’s process of recalibrating its hormonal signals. During this time, individuals may notice changes in symptoms such as cramping, breast tenderness, or mood swings, which can be unsettling. Keeping a detailed log of menstrual cycles, symptoms, and any lifestyle changes can be beneficial for understanding one’s unique recovery process and can provide valuable insights for healthcare providers if further assistance is needed.
Moreover, lifestyle factors such as diet, exercise, and stress management can significantly influence the recovery of the menstrual cycle. Engaging in regular physical activity, maintaining a balanced diet rich in nutrients, and practicing stress-reduction techniques like yoga or meditation can help support hormonal balance during this transitional period. It’s essential to approach this time with patience and self-care, as the body navigates the complexities of hormonal reestablishment.
Factors Affecting Cycle Return
Several factors can influence how quickly menstrual cycles return after stopping birth control. These include individual health conditions, lifestyle choices, and environmental influences that affect hormonal balance and reproductive health.

Pre-Existing Conditions That May Delay Recovery
Underlying medical conditions can significantly impact the return of menstrual cycles. Polycystic ovary syndrome (PCOS), thyroid disorders, and other hormonal imbalances are common culprits that may delay or disrupt the resumption of regular periods.
PCOS, for example, affects up to 10% of women of reproductive age and is characterized by irregular or absent ovulation, elevated androgen levels, and polycystic ovaries. For individuals with PCOS, stopping birth control may unmask or exacerbate symptoms, leading to prolonged menstrual irregularities. The hormonal fluctuations associated with PCOS can also result in additional symptoms such as weight gain, acne, and excessive hair growth, further complicating the overall health picture.
Thyroid dysfunction, including hypothyroidism and hyperthyroidism, can also interfere with menstrual cycles. The thyroid gland plays a critical role in regulating metabolism and hormonal balance, and its dysfunction can lead to amenorrhea (absence of menstruation) or oligomenorrhea (infrequent menstruation). Women with thyroid issues may experience a range of symptoms, including fatigue, mood swings, and changes in weight, which can further impact their reproductive health. Regular monitoring and management of thyroid levels are essential for those affected.
Other conditions such as hyperprolactinemia, eating disorders, and significant weight fluctuations can further complicate the return of normal cycles. Hyperprolactinemia, characterized by elevated levels of prolactin, can inhibit ovulation and lead to irregular periods. Eating disorders, particularly those involving restrictive eating or excessive exercise, can disrupt the delicate balance of hormones necessary for regular menstruation. It is essential to consider these factors when evaluating delayed menstrual return.
Lifestyle and Environmental Influences
Lifestyle factors, including stress, diet, exercise, and environmental exposures, can profoundly affect hormonal health and menstrual regularity. Chronic stress, for instance, elevates cortisol levels, which can suppress the HPO axis and delay ovulation. This stress response can create a cycle of anxiety and hormonal imbalance, making it difficult for the body to regain its natural rhythm.
Intense physical activity or sudden changes in exercise routines can also disrupt menstrual cycles. Athletes or individuals engaging in high levels of physical exertion may experience amenorrhea due to energy deficits and hormonal imbalances. The type of exercise matters. Excessive training without adequate recovery can lead to a condition known as the female athlete triad. This condition encompasses disordered eating, menstrual dysfunction, and decreased bone density.
Nutrition plays a vital role as well. Deficiencies in essential nutrients like vitamin D, iron, and healthy fats can impair hormone synthesis and regulation. A balanced diet rich in whole foods, including fruits, vegetables, lean proteins, and healthy fats, supports overall hormonal health. Exposure to endocrine-disrupting chemicals may interfere with reproductive hormones and prolong cycle irregularities. Awareness of these environmental factors can empower individuals to make healthier choices that promote hormonal balance and menstrual regularity.
Managing Delayed Menstrual Return
Experiencing a delay in the return of menstrual cycles can be concerning. Especially for those trying to conceive or maintain reproductive health. Understanding when to seek medical advice and exploring natural approaches to support hormonal balance can help manage this transition effectively.
When to Consult a Healthcare Provider
If menstrual cycles do not return within three to six months after stopping birth control, it is advisable to consult a healthcare provider. Persistent amenorrhea or irregular cycles warrant evaluation to rule out underlying medical conditions or hormonal imbalances.
A healthcare provider may perform a thorough medical history, physical examination, and laboratory tests to assess hormone levels, thyroid function, and other relevant markers. In some cases, imaging studies such as pelvic ultrasound may be necessary to evaluate ovarian and uterine health.
Early consultation can help identify treatable conditions and provide guidance on fertility planning or hormonal therapies if needed. The U.S. Office on Women’s Health recommends seeking medical advice if periods have not returned within three months after stopping hormonal contraception or if there are other concerning symptoms such as severe pain or abnormal bleeding.
Additionally, understanding the psychological impact of delayed menstrual return is crucial. Many individuals may experience anxiety or distress regarding their reproductive health, which can further complicate hormonal regulation. Engaging in open conversations with healthcare providers about emotional well-being can lead to a more holistic approach to treatment, addressing both physical and mental health aspects.
Natural Approaches to Support Hormonal Balance
While medical evaluation is essential for persistent issues, several natural strategies can support the body’s hormonal recovery after stopping birth control. Prioritizing stress management through mindfulness, yoga, or meditation can reduce cortisol levels and promote hormonal equilibrium.
Maintaining a balanced diet rich in whole foods, healthy fats, and adequate protein supports hormone production. Incorporating foods high in antioxidants, such as berries and leafy greens, can reduce inflammation and improve overall reproductive health.
Regular, moderate exercise helps regulate hormones and improve insulin sensitivity, which is particularly beneficial for individuals with PCOS. However, it is important to avoid excessive exercise that may exacerbate menstrual irregularities.
Herbal supplements like Vitex agnus-castus (chasteberry) have been traditionally used to support menstrual regularity, but it is crucial to consult a healthcare provider before starting any supplements, especially if other medical conditions are present.
Ensuring adequate sleep and minimizing exposure to endocrine disruptors can further aid in restoring hormonal balance. Sleep hygiene practices, such as maintaining a consistent sleep schedule and creating a restful environment, are essential for overall hormonal health.
In addition to these lifestyle changes, fostering a supportive social network can be beneficial. Sharing experiences with friends or joining support groups can provide emotional comfort and practical advice. This makes the journey through hormonal fluctuations feel less isolating. Engaging with communities that focus on reproductive health is also helpful. It can empower individuals with knowledge and resources to navigate their unique situations.
Menstrual cycles after stopping birth control varies widely among individuals due to hormonal regulation, pre-existing conditions, and lifestyle factors. Understanding these influences and knowing when to seek professional advice can help manage expectations and support reproductive health during this transitional period.