Discover the potential benefits and side effects of HCG injections for men in this comprehensive article.
HCG Injection for Male: Benefits and Side Effects
In recent years, Human Chorionic Gonadotropin injections have gained popularity as a treatment option for men. These injections, also known as Human Chorionic Gonadotropin injections, offer several benefits for men’s health. However, it is important to be aware of the potential side effects and precautions associated with this treatment. In this article, we will take a closer look at the understanding of Human Chorionic Gonadotropin injections, their benefits, side effects, administration methods, and contraindications.
Understanding HCG
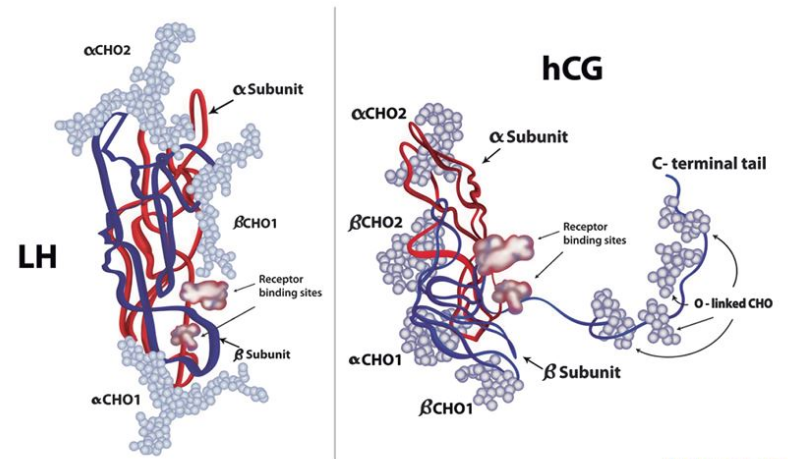
Before diving into the benefits and side effects of HCG injections, also known as trigger shots, let’s first understand what HCG is. HCG, or Human Chorionic Gonadotropin, is a hormone naturally produced in the human body. It is typically associated with pregnancy as it is responsible for supporting the growth and development of the fetus.
What is HCG?
HCG is a glycoprotein hormone that is produced by the placenta during pregnancy. Its primary function is to stimulate the production of progesterone, which is essential for maintaining a healthy pregnancy. HCG also helps regulate the metabolism and hormone production in both men and women.
The Role of HCG in the Male Body
HCG plays a crucial role in the male body by stimulating the production of testosterone, the primary male sex hormone. Testosterone is responsible for various male characteristics, including muscle development, bone density, and libido. By increasing testosterone levels, trigger shots can potentially provide several benefits for men’s health.
It’s important to note that people use these injections with certain weight loss programs. The theory behind this approach is that HCG can help suppress appetite and promote fat loss when used in conjunction with a low-calorie diet. However, the efficacy of this method is a topic of debate among healthcare professionals, with some questioning its scientific basis.
Potential Side Effects of HCG
While HCG is generally considered safe when administered under medical supervision, there are potential side effects to be aware of. These can include headache, fatigue, irritability, and swelling at the injection site. In rare cases, more serious side effects such as blood clots and allergic reactions may occur. It’s crucial to discuss the risks and benefits of HCG with a healthcare provider before starting this treatment.
The Benefits of HCG for Men
Now let’s explore some of the specific benefits that HCG can offer for men:
Boosting Testosterone Levels
One of the key benefits of HCG is their ability to boost testosterone levels in men. Low testosterone levels can lead to various symptoms, including fatigue, decreased libido, and mood swings. By increasing testosterone production, HCG can help improve these symptoms and enhance overall well-being.
Fertility Enhancement
HCG is also commonly used to treat fertility issues in men. They can help stimulate the production of sperm and increase sperm count, improving the chances of conception. For men trying to treat infertility, HCG may offer a promising solution.
Weight Loss and Muscle Gain
In addition to its hormonal benefits, HCG have gained attention for their potential in promoting weight loss and muscle gain. Some men have reported significant improvements in body composition and athletic performance after undergoing HCG therapy. However, it is important to note that individual results may vary, and HCG should not be considered as a substitute for a healthy diet and exercise regimen.
Furthermore, HCG is been found to have anti-inflammatory properties, which can be beneficial for men dealing with conditions such as arthritis or muscle soreness. The reduction in inflammation can lead to improved joint health and mobility, allowing men to engage in physical activities with greater ease and comfort.
Another lesser-known benefit of HCG for men is their potential to improve cognitive function. Research suggests that HCG may have neuroprotective effects, helping to enhance memory, focus, and overall brain health. This cognitive enhancement can be particularly valuable for men experiencing age-related cognitive decline or seeking to optimize their mental performance.
The Side Effects of HCG for Men
While Human Chorionic Gonadotropin injections can offer various benefits, it is important to be aware of the potential side effects associated with this treatment:
Human Chorionic Gonadotropin (HCG) injections are commonly used in men to treat low testosterone levels, improve fertility, and aid when you’re trying to lose weight. These injections work by mimicking the hormone LH (luteinizing hormone), which stimulates the testes to produce more testosterone. However, like any medication, HCG can have side effects that vary in severity from person to person.
Common Side Effects
Some men may experience common side effects such as acne, mood swings, and fluid retention while undergoing HCG therapy. These side effects are generally mild and subside over time. However, if any of these symptoms persist or worsen, it is crucial to seek medical advice.
Another common side effect of Human Chorionic Gonadotropin injections in men is testicular shrinkage. This occurs because the body may interpret the presence of exogenous HCG as a signal to decrease natural testosterone production, leading to a temporary reduction in testicular size. It is important to note that testicular shrinkage is usually reversible once HCG therapy is discontinued.
Potential Long-Term Risks
Although rare, there are potential long-term risks associated with HCG. These include the development of blood clots, gynecomastia (enlarged breast tissue), and prostate enlargement. It is important to discuss these risks with a healthcare professional before starting HCG therapy.
Furthermore, some studies have suggested a possible link between prolonged HCG use and an increased risk of developing certain types of cancer, such as prostate cancer. While more research is needed to establish a definitive connection, individuals considering long-term HCG therapy should be aware of this potential risk and discuss it with their healthcare provider.
Administering HCG Injections
When it comes to administering trigger shots, there are a few important considerations to keep in mind:
Human Chorionic Gonadotropin (HCG) injections are commonly used for various purposes, such as fertility treatments and weight loss programs. The hormone HCG is produced naturally in the body during pregnancy and can also be administered synthetically for medical reasons. It is crucial to understand the specific purpose for which the injections are being prescribed and how they function within the body.
Dosage and Frequency
The dosage and frequency of Human Chorionic Gonadotropin injections may vary depending on the individual’s specific needs and medical history. It is essential to follow the prescribed dosage and schedule provided by a qualified healthcare professional. Deviating from the recommended dosage can have adverse effects on the body.
It is important to note that the dosage of HCG for weight loss may differ from those used in fertility treatments. Weight loss protocols often involve lower doses of trigger shots administered alongside a low-calorie diet, while fertility treatments may require higher doses at specific times during a woman’s menstrual cycle.
Self-Administration vs. Professional Administration
HCG injections can be self-administered or administered by a healthcare professional. While self-administration may offer convenience and cost-effectiveness, it is crucial to receive proper training and guidance to ensure correct technique and minimize the risk of complications. Consulting with a healthcare professional is recommended for those who are unsure about the proper administration method.
For individuals opting for self-administration of trigger shots, it is essential to learn the proper techniques for preparing the injection, choosing the right injection site, and ensuring sterile practices to prevent infections. Healthcare providers can offer guidance on these aspects and address any concerns or questions that may arise during the self-administration process.
Contraindications and Precautions
While Human Chorionic Gonadotropin injections can provide significant benefits for men, there are certain situations where caution should be exercised:
When HCG Injections Should be Avoided
Individuals with a history of prostate cancer, breast cancer, or other hormonally-driven cancers should avoid Human Chorionic Gonadotropin injections. It is crucial to discuss any pre-existing medical conditions with a healthcare professional before considering HCG therapy.
Precautions to Take Before Starting HCG Injections
Prior to starting trigger shots, it is important to undergo a thorough medical evaluation. This evaluation may include a comprehensive physical examination, blood tests, and a review of medical history. By conducting these assessments, healthcare professionals can identify any potential risks or contraindications and tailor the treatment plan accordingly.
During the physical examination, the healthcare professional will assess various aspects of your health, including your blood pressure, heart rate, and overall physical fitness. They may also examine your testicles for any abnormalities or signs of underlying conditions. This comprehensive evaluation allows the healthcare professional to have a complete picture of your health status and determine if HCG therapy is appropriate for you.
In addition to the physical examination, blood tests are an essential part of the evaluation process. These tests help measure hormone levels, including testosterone, estrogen, and other relevant markers. By analyzing these results, healthcare professionals can identify any hormonal imbalances or abnormalities that may impact the effectiveness or safety of HCG therapy.
Furthermore, a review of your medical history is crucial in determining whether HCG injections are suitable for you. This includes discussing any previous treatments, surgeries, or medications you have taken. It is important to disclose all relevant information to your healthcare professional to ensure they have a comprehensive understanding of your health background.
In conclusion, HCG injections offer several benefits for men’s health, including increased testosterone levels, fertility enhancement, and potential improvements in weight loss and muscle gain. However, it is crucial to be aware of the potential side effects and precautions associated with this treatment. By understanding the role of HCG in the male body, administering injections correctly, and taking necessary precautions, men can make informed decisions about whether HCG therapy is suitable for them. Consulting with a qualified healthcare professional is essential to ensure safe and effective treatment.