Uncovering Fertility Myths
In today’s society, there are countless misconceptions and myths surrounding fertility. Many individuals are often misinformed, leading to unnecessary worry and confusion. It is essential to debunk these fertility myths and provide accurate information to help individuals make informed decisions. In this article, we will be uncovering the truth behind age and fertility, myths about diet and its impact on reproductive health, understanding male fertility, the role of stress in fertility, the influence of weight on fertility, natural remedies for fertility, and the impact of birth control on future fertility.
The Truth Behind Age and Fertility
One of the most prevalent fertility myths is the belief that women can conceive at any age without any difficulty. However, the truth is that a woman’s fertility gradually declines after her mid-20s and significantly decreases in her late 30s and 40s. While it is still possible to get pregnant at an older age, the chances of success decrease, and the risk of complications, such as miscarriage and birth defects, increases.
Additionally, men’s fertility also declines with age, although not as steeply as women’s. Advanced paternal age can lead to a higher risk of genetic abnormalities and certain health conditions in offspring. It is important for individuals to understand the impact of age on fertility when planning for a family.
It’s important to note that there are various factors that can affect fertility besides age. Lifestyle choices, such as smoking, excessive alcohol consumption, and poor diet, can also have a significant impact on fertility for both men and women. Maintaining a healthy lifestyle, including regular exercise and a balanced diet, can help improve fertility outcomes.
Furthermore, seeking guidance from a fertility specialist can provide valuable insights into individual fertility health. Fertility tests can help assess reproductive potential and identify any underlying issues that may affect conception. By being proactive and informed about fertility, individuals can make empowered decisions when planning for their future family.
Myths About Diet and Its Impact on Reproductive Health
There are several myths surrounding diet and its impact on fertility. One common myth is that consuming certain foods or supplements can significantly boost fertility. While a healthy diet is important for overall reproductive health, there is no magical food or supplement that can guarantee pregnancy.
However, maintaining a balanced diet, rich in fruits, vegetables, whole grains, and lean proteins, can support reproductive health and increase the chances of conception. It is important to consult with a healthcare professional or a fertility specialist to understand any specific dietary recommendations for fertility.
Another misconception is that weight has a direct correlation with fertility. While being underweight or overweight can impact fertility, it is not solely determined by weight. Factors such as hormone levels, stress, and underlying medical conditions also play a crucial role in reproductive health.
Furthermore, certain lifestyle habits like smoking, excessive alcohol consumption, and lack of physical activity can negatively affect fertility. It is essential to adopt a healthy lifestyle that includes regular exercise, adequate sleep, and stress management techniques to optimize reproductive health.
Understanding Male Fertility: What You Need to Know
Fertility discussions often focus primarily on women, but it is essential to understand male fertility as well. Many myths surround male fertility, including the belief that men are fertile indefinitely. However, men also experience a decline in fertility as they age.
Other factors, such as lifestyle choices, stress, and exposure to toxins, can also impact male fertility. Understanding the basics of male reproductive health, including factors that can affect sperm quality and quantity, is crucial for couples trying to conceive.
One crucial aspect of male fertility that is often overlooked is the role of temperature. The testes, where sperm production occurs, are located outside the body in the scrotum because sperm production requires a slightly lower temperature than the body’s core. Tight clothing, hot tubs, and laptops placed directly on the lap can all increase scrotal temperature, potentially impacting sperm quality.
Furthermore, it’s important to note that certain medical conditions and medications can also affect male fertility. Conditions such as varicoceles (enlarged veins within the scrotum) or hormonal imbalances can interfere with sperm production. Additionally, some medications, including anabolic steroids and certain antidepressants, have been linked to decreased sperm production or quality.
The Role of Stress in Fertility: Separating Fact from Fiction
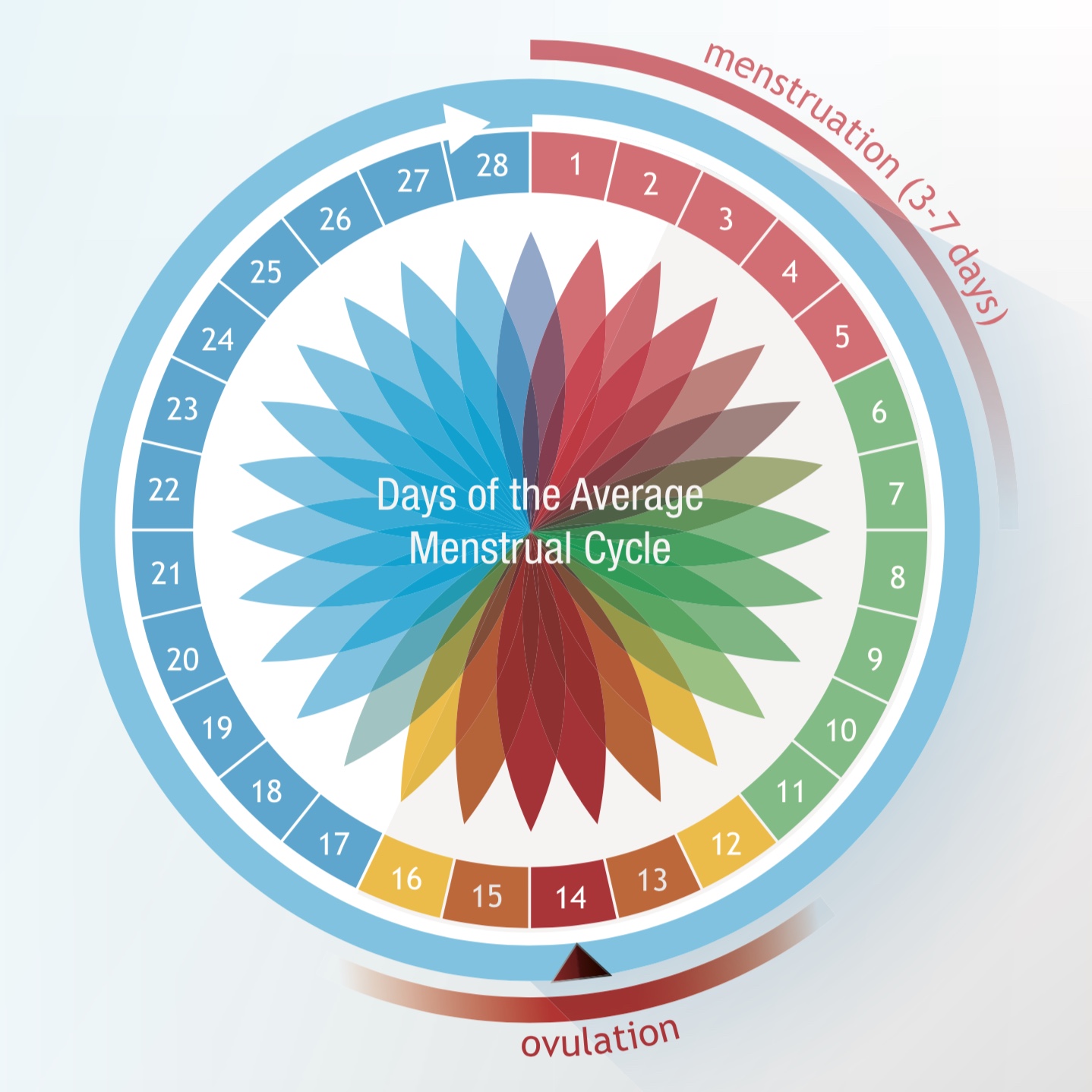
Stress has long been associated with infertility, leading to the belief that relaxation alone can enhance fertility. While excessive stress can disrupt hormonal balance and the menstrual cycle, the relationship between stress and fertility is complex.
While reducing stress is beneficial for overall well-being, it is unlikely to be a stand-alone solution for fertility issues. It is important to investigate other potential factors and consult with medical professionals to address any fertility concerns.
Research has shown that stress can impact both male and female fertility. In women, high levels of stress can lead to irregular menstrual cycles, making it difficult to predict ovulation. For men, stress can affect sperm quality and quantity, potentially reducing the chances of conception.
Moreover, the connection between stress and fertility is not solely biological. Psychological factors, such as anxiety and depression, can also play a role in fertility outcomes. Stress management techniques, such as mindfulness meditation and yoga, may help individuals cope with the emotional toll of infertility, improving overall mental health.
The Influence of Weight on Fertility: What Science Says
Another common fertility myth revolves around weight and its impact on fertility. Some individuals believe that being underweight or overweight can hinder the ability to conceive. While weight does play a role in fertility, it is not the sole determining factor.
Being significantly underweight or overweight can disrupt hormone balance and menstrual cycles, making it more difficult to conceive. Achieving a healthy weight through balanced nutrition and regular exercise can improve fertility outcomes.
Research has shown that women who are underweight may have irregular periods or stop ovulating altogether, which can reduce their chances of getting pregnant. On the other hand, obesity can lead to insulin resistance and hormonal imbalances, affecting the quality of eggs and sperm. These issues can make it harder for couples to conceive naturally.
It’s important to remember that weight is just one piece of the puzzle when it comes to fertility. Factors such as age, overall health, and genetics also play significant roles in determining a person’s reproductive health. Seeking guidance from a healthcare provider or fertility specialist can help individuals understand how weight may be impacting their fertility and what steps they can take to improve their chances of conceiving.
Natural Remedies for Fertility: What Works and What Doesn’t
With the increasing popularity of natural remedies, many individuals turn to alternative therapies to boost fertility. However, it is crucial to differentiate between evidence-based interventions and unsupported claims.
Some natural remedies, such as acupuncture and certain herbal supplements, may have a positive impact on fertility when used in conjunction with conventional treatments. However, it is essential to consult with a fertility specialist before incorporating any natural remedies into a fertility journey.
Acupuncture, an ancient Chinese practice, is believed to help regulate the body’s energy flow, known as Qi, which can in turn improve reproductive health. By stimulating specific points on the body with thin needles, acupuncture aims to promote blood flow to the reproductive organs and balance hormone levels. While research on acupuncture’s effectiveness in enhancing fertility is ongoing, many individuals have reported increased relaxation and reduced stress levels after acupuncture sessions.
In addition to acupuncture, certain herbal supplements like chasteberry, maca root, and evening primrose oil are often touted for their potential fertility-boosting properties. Chasteberry, for example, is thought to help regulate menstrual cycles and balance hormones, while maca root is believed to support overall reproductive health. Evening primrose oil, rich in omega-6 fatty acids, is said to promote cervical mucus production, which can aid in conception. It is important to note, however, that the efficacy of these herbal supplements varies from person to person, and consulting a healthcare provider is recommended to ensure they are safe and appropriate for individual needs.
The Impact of Birth Control on Future Fertility
There is a widespread misconception that using birth control methods, such as the pill or IUD, can permanently damage future fertility. However, the truth is that the effects of birth control on fertility are temporary.
Once a person stops using birth control methods, such as hormonal contraceptives, fertility typically returns to its previous state. While some individuals may experience a brief delay in conceiving after discontinuing birth control, it does not cause long-term infertility.
It is important to understand the facts surrounding birth control methods to make informed decisions about family planning.
Furthermore, it is worth noting that certain types of birth control, such as the copper IUD, do not contain hormones and therefore do not have any impact on future fertility once removed. This non-hormonal option provides a safe and effective contraceptive method for individuals concerned about hormonal influences on their bodies.
Additionally, consulting with a healthcare provider can help individuals explore the wide range of birth control options available and find the one that best suits their needs and future fertility goals. By understanding the mechanisms of different birth control methods and their effects on fertility, individuals can make empowered choices regarding their reproductive health.
Conclusion
Dispelling fertility myths is essential in empowering individuals to make educated choices about their reproductive health. By understanding the truth behind age and fertility, the impact of diet, male fertility, stress, weight, natural remedies, and birth control on fertility, individuals can navigate their fertility journey with confidence.
Remember, consulting with a healthcare professional or a fertility specialist is key to obtaining personalized guidance and support throughout the process. By debunking myths and embracing accurate information, individuals can make informed decisions and take actions that increase their chances of building the family they desire.