Learn the key differences between OBGYNs and REIs
What is the difference between OB/GYN and REI?
When it comes to women’s healthcare, there are a variety of specialists to choose from. Two common specialties are OBGYN (Obstetrician-Gynecologist) and REI (Reproductive Endocrinology and Infertility) physicians. While both focus on women’s reproductive health, there are important differences between the two that can greatly impact your healthcare needs. In this article, we will explore the key differences in training and specialization, when to see an OBGYN for routine care and beyond, the role of REI in infertility and reproductive health, common conditions treated by OBGYNs and REIs, and how to choose the right specialist for your needs.
Key Differences in Training and Specialization
Let’s start by understanding the training and specialization differences between OBGYNs and REIs. OBGYNs are medical doctors who specialize in both obstetrics (pregnancy and childbirth) and gynecology (women’s reproductive health). After completing medical school, OBGYNs undergo a four-year residency program where they gain experience in various aspects of women’s health. They are trained to provide general care, perform surgical procedures, and manage pregnancy and childbirth. OBGYNs play a crucial role in women’s healthcare. They offer a wide range of services from annual check-ups to delivering babies via vaginal or cesarean birth.
On the other hand, REIs undergo additional training beyond OBGYN residency. They specialize in the management of infertility and reproductive endocrinology, which involves the hormonal aspects of reproductive health. REIs are highly skilled in diagnosing and treating complex reproductive disorders that may hinder a couple’s ability to conceive. They work closely with patients to explore various fertility treatment options. These include in vitro fertilization (IVF) and intrauterine insemination (IUI), to help them achieve their dream of starting a family.
REIs typically complete a three-year fellowship program in reproductive endocrinology and infertility after their OBGYN residency. During this fellowship, they gain expertise in diagnosing and treating infertility, hormonal imbalances, and conditions related to reproductive health. This additional training allows REIs to provide specialized care for women struggling with fertility issues and hormonal disorders. They also conduct research to advance the field of reproductive medicine. Thus contributing to new breakthroughs in fertility treatments and technologies that benefit patients worldwide.

When to See an OBGYN: Routine Care and Beyond
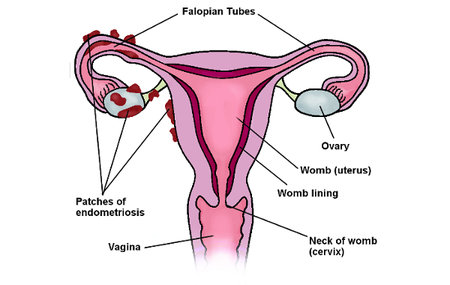
For routine care and general women’s health concerns, an OBGYN is often the first point of contact. OBGYNs provide a wide range of preventive care, including annual well-woman exams, Pap smears, and contraceptive counseling. They can also diagnose and treat common gynecological conditions such as menstrual irregularities, urinary tract infections, and vaginal infections. OBGYNs are skilled in performing various procedures. These procedures include colposcopy to examine abnormal cervical cells and endometrial biopsy to evaluate abnormal uterine bleeding.
Additionally, OBGYNs play a vital role in managing pregnancy and childbirth. They provide prenatal care, monitor fetal development, and guide women through the delivery process. OBGYNs are trained to handle both low-risk and high-risk pregnancies and can perform cesarean section deliveries if necessary. They also offer postpartum care to ensure the well-being of both mother and baby.
Furthermore, OBGYNs are also equipped to address reproductive health issues beyond pregnancy and routine care. They can assist with fertility evaluations and treatments for couples struggling with infertility. OBGYNs are knowledgeable about various contraceptive options. They can help individuals choose the most suitable method based on their health needs and preferences. Additionally, they are trained to diagnose and manage conditions such as polycystic ovary syndrome (PCOS), endometriosis, and fibroids.
Moreover, OBGYNs are advocates for women’s health and wellness, promoting regular screenings for breast and ovarian cancers. They educate patients on the importance of self-breast exams and can perform clinical breast exams to detect any abnormalities. OBGYNs stay up-to-date on the latest research and guidelines in women’s health. They provide evidence-based care and empower their patients to make informed decisions about their health.
The Role of REI in Infertility and Reproductive Health
When facing difficulties in conceiving a child or managing complex reproductive health issues, a consultation with an REI is crucial. REIs specialize in diagnosing and treating infertility in both men and women. They conduct thorough assessments to identify underlying causes of infertility and develop personalized treatment plans. REIs are skilled in various advanced reproductive technologies. These include in vitro fertilization (IVF), intrauterine insemination (IUI), and preimplantation genetic testing (PGT). These can increase the chances of pregnancy for couples struggling with infertility.
Furthermore, REIs provide comprehensive care for hormonal disorders, including polycystic ovary syndrome (PCOS), endometriosis, and premature ovarian insufficiency (POI). They offer hormonal therapies to regulate menstrual cycles, manage symptoms, and preserve fertility when necessary. REIs also play a crucial role in fertility preservation for individuals undergoing cancer treatment or other medical procedures that may compromise fertility.
It is important to note that REIs work closely with a multidisciplinary team of healthcare professionals to provide holistic care to patients. This collaborative approach ensures that individuals receive comprehensive support throughout their fertility journey. Addressing not only the physical aspects but also the emotional and psychological challenges that may arise.
Moreover, REIs stay abreast of the latest advancements in reproductive medicine through ongoing research and participation in clinical trials. This dedication to continuous learning and innovation enables REIs to offer cutting-edge treatments and technologies to their patients. This ultimately improves success rates and outcomes in assisted reproductive techniques. By combining expertise, compassion, and innovation, REIs play a vital role in helping individuals and couples achieve their dream of starting or expanding their families.
Common Conditions Treated by OBGYNs and REIs
Both OBGYNs and REIs are integral parts of women’s healthcare. They specialize in diagnosing and treating a wide range of conditions related to reproductive health. OBGYNs play a crucial role in managing conditions such as uterine fibroids, which are non-cancerous growths in the uterus that can cause heavy periods and pelvic pain. They also commonly address ovarian cysts, fluid-filled sacs that can develop on the ovaries and sometimes lead to discomfort or complications.
Moreover, OBGYNs are skilled in treating pelvic inflammatory disease (PID), an infection of the female reproductive organs often caused by sexually transmitted bacteria. This condition can result in pelvic pain, infertility, and other serious complications if left untreated. Additionally, OBGYNs assist patients dealing with urinary incontinence, a common issue among women that can significantly impact quality of life. They offer various treatment options, including lifestyle changes, pelvic floor exercises, and in some cases, surgical interventions.
On the other hand, Reproductive Endocrinologists (REIs) specialize not only in addressing infertility and hormonal disorders but also in managing complex reproductive issues. They are equipped to help patients facing recurrent pregnancy loss, a heartbreaking experience that can be caused by various factors such as genetic abnormalities, hormonal imbalances, or uterine issues. Furthermore, REIs are well-versed in genetic disorders that can impact reproductive health, offering counseling and treatment options for individuals with conditions that may affect their fertility or pregnancy outcomes.
REIs work closely with OBGYNs and other healthcare providers to deliver personalized care plans that consider each patient’s specific circumstances and goals. By collaborating with a multidisciplinary team, they ensure that individuals receive comprehensive and holistic care that addresses all aspects of their reproductive health. This collaborative approach allows for a more integrated and effective treatment strategy, ultimately leading to better outcomes for patients facing complex reproductive challenges.
How to Choose the Right Specialist for Your Needs
Choosing between an OBGYN and an REI depends on your specific healthcare needs. If you are seeking routine preventive care or are planning to start a family in the future, an OBGYN is an excellent choice. They will guide you through each stage of pregnancy and provide comprehensive gynecological care.
However, if you are experiencing fertility issues, have irregular menstrual cycles, or require specific expertise in reproductive endocrinology matters, consulting with an REI is crucial. REIs focus on diagnosing and treating complex reproductive conditions, offering a range of advanced fertility treatments.
Ultimately, the decision may also depend on personal preference and communication with potential healthcare providers. It is important to choose a specialist who not only has the necessary expertise but also makes you feel comfortable and supported throughout your healthcare journey.
Conclusion
By understanding the training, specialization, and roles of OBGYNs and REIs, women can make informed decisions about their healthcare. Whether seeking routine care or facing fertility challenges, these specialists play integral roles in women’s reproductive health. By collaborating with these experts, women can receive the personalized care they need to navigate the various phases of their reproductive journey.
When considering whether to consult with an OBGYN or an REI, it’s essential to delve deeper into the differences in their training and expertise. OBGYNs undergo extensive training in obstetrics and gynecology, focusing on women’s reproductive health, pregnancy, and childbirth. They are equipped to handle a wide range of issues, from annual exams and contraception counseling to managing high-risk pregnancies.
On the other hand, REIs are subspecialists within the field of obstetrics and gynecology who have completed additional training in reproductive endocrinology and infertility. They possess advanced knowledge in diagnosing and treating conditions that affect fertility, such as polycystic ovary syndrome (PCOS), endometriosis, and male factor infertility. REIs also offer specialized treatments like in vitro fertilization (IVF) and intrauterine insemination (IUI) to help individuals and couples overcome infertility challenges.