What Is Male Infertility
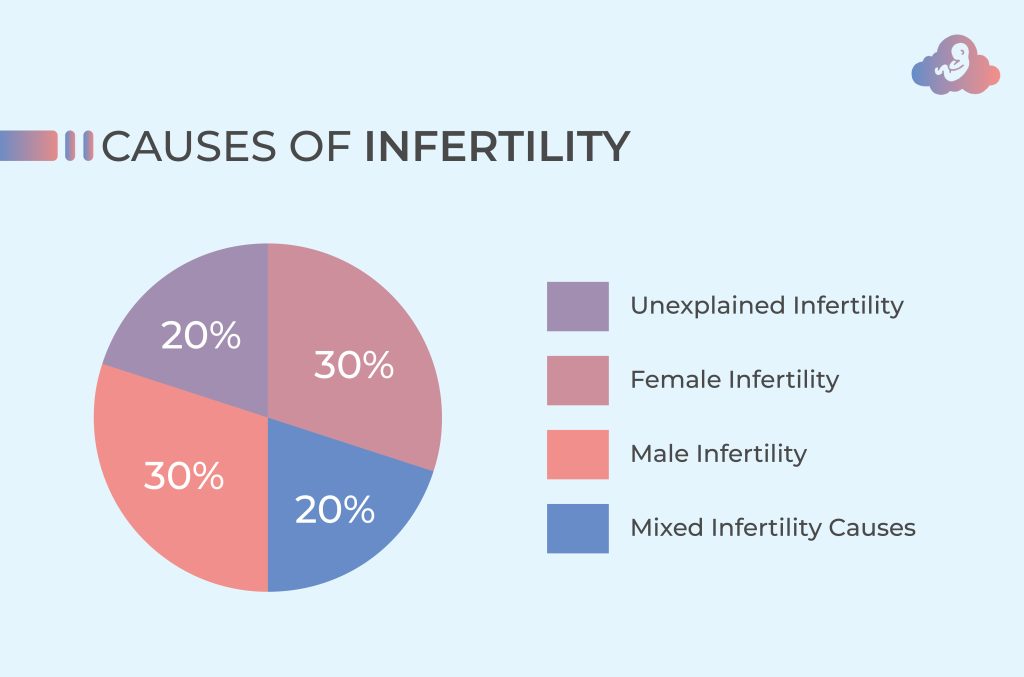
Infertility is a common problem affecting millions of couples worldwide, and male factor infertility is a significant factor in nearly half of all cases. The World Health Organization defines male infertility as the inability to conceive a child despite regular, unprotected sexual intercourse for at least one year. Infertility can be a stressful and frustrating experience for couples, but understanding the causes and treatment options can provide hope and guidance.
In this article, we will discuss infertility in males. in detail, including its causes, diagnosis, and treatment options. We will also explore lifestyle changes that can improve male fertility and offer advice on how to cope with the emotional impact of infertility.
Causes of Male Infertility
Infertility in males can be caused by a variety of factors, including:
- Low Sperm Count: A low sperm count, also known as oligospermia, is the most common cause of infertility. Men with a low sperm count may have difficulty fertilizing their partner’s egg or may not be able to do so at all.
- Abnormal Sperm: Sperm abnormalities, such as misshapen or immobile sperm, can also cause infertility. Abnormal sperm may not be able to swim to the egg or penetrate its outer layer.
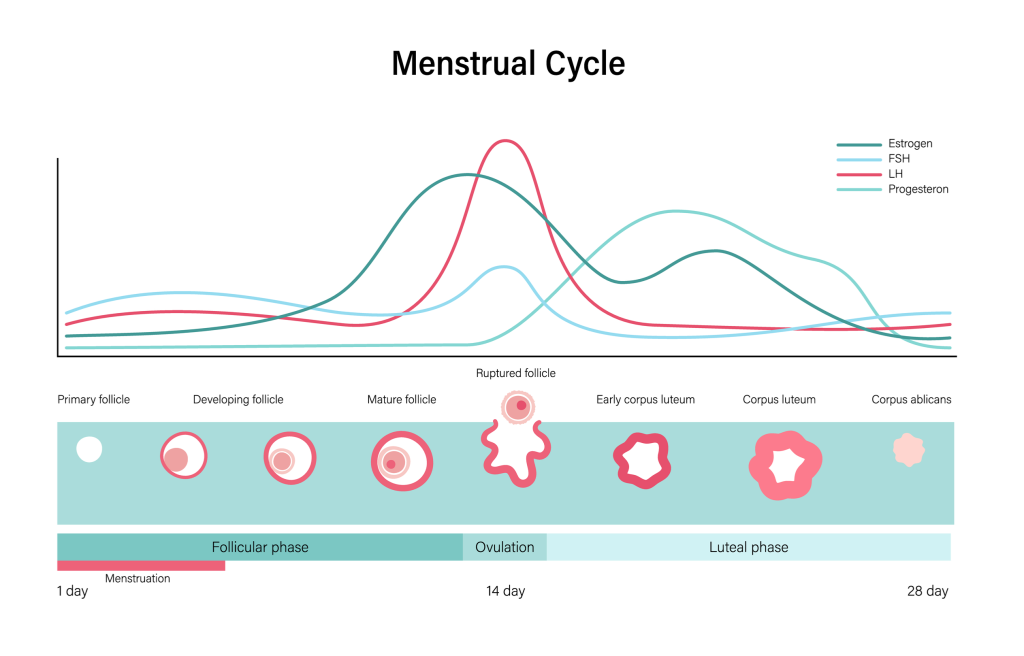
- Hormonal Imbalances: Hormonal imbalances, such as low testosterone levels or high levels of prolactin, can interfere with sperm production and reduce male fertility.
- Varicocele: Varicocele is a swelling of the veins that drain the testicles, which can cause reduced sperm production and quality.
- Genetic Abnormalities: Genetic abnormalities, such as Klinefelter’s syndrome or Y chromosome deletions, can affect sperm production and lead to infertility.
- Infections: Certain infections, such as chlamydia and gonorrhea, can damage the male reproductive system and affect fertility.
- Environmental Factors: Exposure to environmental toxins, such as pesticides and chemicals, can reduce sperm count and quality.
- Lifestyle Factors: Lifestyle factors, such as smoking, excessive alcohol consumption, and drug use, can also reduce male fertility.

Diagnosing Male Infertility
If a couple has been trying to achieve pregnancy for at least a year without success, it may be time to seek medical help. A doctor can perform a physical exam and conduct a variety of tests to diagnose infertility, including:
- Semen Analysis: A semen analysis is a simple and non-invasive test that can determine the quality and quantity of sperm in the semen.
- Hormone Testing: Hormone testing can check for imbalances that may be affecting sperm production.
- Genetic Testing: Genetic testing can detect any abnormalities that may be affecting fertility.
- Imaging Tests: Imaging tests, such as ultrasound or MRI, can detect structural abnormalities in the male reproductive system.
- Testicular Biopsy: In some cases, a testicular biopsy may be necessary to diagnose infertility.
Treatment Options for Male Infertility
Treatment options for infertility depend on the underlying cause of the problem. Some common treatment options include:
- Medications: Medications can be prescribed to correct hormonal imbalances, improve sperm production, or treat infections.
- Surgery: Surgery may be necessary to repair structural abnormalities, such as a varicocele.
- Assisted Reproductive Techniques: Assisted reproductive techniques, such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI), can be used to overcome infertility.
- Lifestyle Changes: Lifestyle changes, such as quitting smoking, reducing alcohol consumption, and maintaining a healthy weight, can improve male fertility.
Coping with Male Infertility
Infertility can be a challenging and emotional experience for couples, but there are several ways to cope with the stress and frustration of infertility. Here are some tips for coping with infertility in males:
- Seek Support: Talk to your partner, friends, or family about your feelings. Consider joining a support group for couples dealing with infertility.
- Practice Self-Care: Take care of your physical and emotional health by eating well, exercising regularly, and engaging in stress-reducing activities, such as yoga or meditation.
- Be Open to Alternative Paths to Parenthood: Consider alternative paths to parenthood, such as adoption or donor insemination.
- Take a Break: Take a break from trying to conceive if you need it. It’s important to take time for yourself and your relationship.
- Get Professional Help: If you’re struggling to cope with infertility, consider seeking professional help from a therapist or counselor.
Preventing Male Infertility
While not all cases of infertility can be prevented, there are some steps men can take to improve their fertility and reduce their risk of infertility:
- Maintain a Healthy Weight: Being overweight or obese can affect sperm production and quality. Maintaining a healthy weight can help improve male fertility.
- Quit Smoking: Smoking can reduce sperm count and quality. Quitting smoking can improve male fertility.
- Limit Alcohol and Drug Use: Excessive alcohol consumption and drug use can also affect male fertility. Limiting alcohol and drug use can help improve fertility.
- Avoid Environmental Toxins: Exposure to environmental toxins, such as pesticides and chemicals, can reduce sperm count and quality. Avoiding these toxins can help improve male fertility.
Conclusion
Male infertility is a common problem that can be caused by a variety of factors. Understanding the causes and treatment options can provide hope and guidance for couples dealing with infertility. If you are experiencing infertility, talk to your doctor about your options and seek support from loved ones and professionals. By taking steps to improve your fertility and coping with the emotional impact of infertility, you can increase your chances of achieving your dream of becoming a parent.
We strive for accuracy in our fertility information, but remember, every individual’s path is unique. This general guidance might not fit your specific circumstances. Always consult a licensed medical professional for personalized advice based on your health history.
Beyond medical interventions, natural fertility support is diverse. Stress reduction, a healthy diet, consistent exercise, and sufficient sleep are key. Simple adjustments like mindfulness, yoga, or meditation for stress, and prioritizing good sleep, can boost overall well-being and aid fertility. Always consult a specialist for personalized advice; your unique health and fertility require professional guidance.