Explore the comprehensive guide to understanding azoospermia, covering its causes, symptoms, and various treatment options.
Understanding Azoospermia: Causes, Symptoms, and Treatment Options
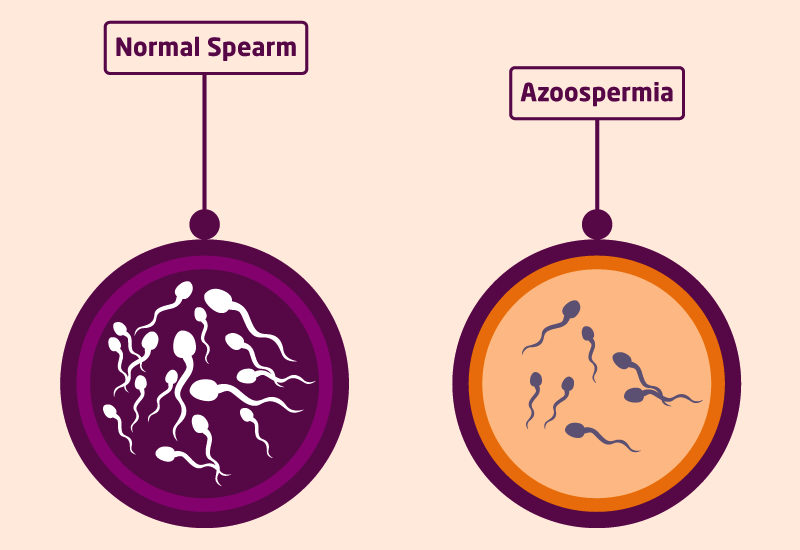
It is a condition that affects male fertility, characterized by the absence of sperm in the ejaculate. In this article, we will delve into the definition, prevalence, causes, symptoms, diagnostic procedures, and treatment options to provide a comprehensive understanding of this condition.
What is Azoospermia?
It refers to the absence of sperm in the semen. Sperm, the male reproductive cells, are essential for fertilizing an egg and achieving successful pregnancy. A complete absence of sperm can make natural conception impossible, requiring alternative methods for achieving parenthood.
It is a condition that can have a significant impact on a man’s fertility and his ability to father a child. It is a complex issue that can be caused by various factors, and understanding its different forms and prevalence is crucial in determining the appropriate treatment options.
Defining Azoospermia
It is classified into two main categories: obstructive and non-obstructive. Obstructive azoospermia occurs due to an obstruction in the reproductive tract, preventing the normal release of sperm. This obstruction can be caused by various factors, such as previous infections, congenital abnormalities, or previous surgeries. On the other hand, non-obstructive azoospermia is attributed to problems within the testicles, resulting in the absence of sperm.
Obstructive azoospermia is generally considered to have a better prognosis. In these cases, the sperm production is usually normal, but the blockage prevents the sperm from reaching the semen. Non-obstructive azoospermia, on the other hand, is often associated with impaired sperm production, which can be caused by genetic factors, hormonal imbalances, or testicular damage.
Prevalence of Azoospermia
Azoospermia affects approximately 1% of all men and around 10-15% of infertile males. It is important to note that it is not a common condition, but its impact on fertility can be significant. Understanding its prevalence can help individuals and couples facing fertility challenges to seek appropriate medical assistance and explore alternative options for achieving parenthood.
There are various factors that can contribute to its development, including genetic disorders, hormonal imbalances, infections, testicular trauma, and certain medical treatments like chemotherapy or radiation therapy. Identifying its underlying cause is crucial in determining the most suitable treatment approach, which may include surgical interventions, hormone therapy, or assisted reproductive techniques such as sperm retrieval and in vitro fertilization (IVF).
It is important for individuals and couples to consult with a fertility specialist who can provide a comprehensive evaluation and guide them through the available treatment options. With advancements in reproductive medicine, there are now more possibilities than ever for individuals to achieve their dream of parenthood.
The Causes of Azoospermia
The absence of sperm in semen, can be caused by various factors, including genetic, lifestyle, environmental, and medical conditions. Understanding these causes is essential for diagnosis and treatment.
Genetic Factors
Genetic abnormalities play a significant role in its development. Chromosomal defects, such as Klinefelter syndrome, where males have an extra X chromosome, can disrupt normal sperm production and function. Similarly, Y-chromosome microdeletions, which involve missing genetic material on the Y chromosome, can also contribute to it.
These genetic factors can have a profound impact on male fertility, affecting the quantity and quality of sperm. Identifying specific genetic abnormalities is crucial for understanding the underlying its cause and developing appropriate treatment strategies.
Lifestyle and Environmental Factors
Lifestyle choices and environmental factors can significantly affect sperm production and quality. Excessive alcohol consumption, smoking, and drug use have been shown to have detrimental effects on male fertility.
Alcohol abuse can disrupt hormone production and impair sperm development, while smoking can damage sperm DNA and reduce sperm motility. Illicit drug use, such as marijuana and cocaine, can also interfere with sperm production and function.
Furthermore, exposure to environmental toxins, such as pesticides, heavy metals, and certain chemicals, can have harmful effects on male reproductive health. These toxins can accumulate in the body over time and disrupt the delicate balance required for normal sperm production.
Adopting a healthy lifestyle, avoiding harmful substances, and minimizing exposure to environmental toxins are essential steps in preventing this condition and maintaining optimal fertility.
Medical Conditions Leading to Azoospermia
Various medical conditions can contribute to the development of azoospermia. Hormonal imbalances, such as low testosterone levels or elevated levels of prolactin, can disrupt the delicate hormonal cascade required for sperm production.
Infections, such as sexually transmitted infections or inflammation of the reproductive organs, can also impair sperm production and function. These infections can cause scarring or blockages in the reproductive tract, preventing the release of sperm during ejaculation.
Testicular trauma, resulting from accidents or injuries, can cause damage to the testicles and disrupt sperm production. Radiation therapy, often used in the treatment of cancer, can also have detrimental effects on sperm production.
Furthermore, certain genetic disorders, such as cystic fibrosis or congenital absence of the vas deferens (CAVD), can cause azoospermia. These conditions affect the structure or function of the reproductive organs, preventing the transport or production of sperm.
It is crucial to identify and address these underlying medical conditions to improve fertility and increase the chances of successful conception. Treatment options may include hormone therapy, surgical interventions, or assisted reproductive techniques, depending on the specific cause of azoospermia.
In conclusion, azoospermia can have various causes, including genetic abnormalities, lifestyle and environmental factors, and medical conditions. Understanding these causes is essential for accurate diagnosis and effective treatment. By addressing the underlying factors, individuals and couples can take proactive steps towards achieving their reproductive goals.
Recognizing the Symptoms of Azoospermia
Azoospermia is primarily asymptomatic, meaning there are no obvious signs or physical discomfort associated with the condition. However, certain emotional and psychological symptoms may arise due to the challenges of infertility.
While the absence of physical symptoms is a defining characteristic of azoospermia, it is important to understand the emotional and psychological impact it can have on individuals and couples. The journey of infertility can be a rollercoaster of emotions, ranging from frustration to sadness, guilt, and anxiety.
For men diagnosed with azoospermia, the news can be devastating. The realization that they may not be able to father a child naturally can lead to feelings of inadequacy and a sense of loss. It is not uncommon for men to question their masculinity and experience a profound sense of grief.
Similarly, women who receive the diagnosis of their partner may also experience a wide range of emotions. They may feel a sense of guilt, blaming themselves for the couple’s infertility, even though it is important to remember that infertility is a shared responsibility. Women may also feel sadness and a deep longing for motherhood, as well as anxiety about the future of their relationship.
It is crucial for individuals and couples facing infertility to seek emotional support and counseling to navigate the challenges associated with the condition. Infertility support groups and therapy sessions can provide a safe space for individuals to express their emotions, share their experiences, and find solace in knowing they are not alone.
Physical Symptoms
As previously mentioned, the absence of sperm is not accompanied by any noticeable physical symptoms and it can only be diagnosed through laboratory tests.
When a couple is trying to conceive and encounters difficulties, it is common for both partners to undergo a series of medical tests to identify the cause of infertility. In the case of azoospermia, a semen analysis is conducted to determine the presence or absence of sperm. This involves collecting a semen sample and examining it under a microscope.
Further diagnostic tests may be necessary to determine the underlying cause. These tests can include hormone level evaluations, genetic testing, testicular biopsies, and imaging studies.
Emotional and Psychological Symptoms
Experiencing azoospermia can evoke a range of emotions, including frustration, sadness, guilt, and anxiety. It is crucial for individuals and couples facing infertility to seek emotional support and counseling to navigate the challenges associated with the condition.
Infertility can put a strain on relationships, as the journey towards parenthood becomes more complex and emotionally demanding. There are stories of couples who experience feelings of isolation and frustration as they navigate the various medical interventions and treatments available.
Furthermore, the societal pressure to have children can exacerbate the emotional toll of infertility. Couples may feel judged or misunderstood by friends, family, and even strangers who do not fully grasp the complexities of their situation.
It is important for individuals and couples to prioritize their mental well-being as they navigate the challenges of azoospermia. Seeking professional help from therapists or counselors who specialize in infertility can provide valuable guidance and support. Additionally, joining support groups or online communities can create a sense of belonging and provide a platform for sharing experiences and coping strategies.
Diagnostic Procedures for Azoospermia
To diagnose azoospermia, healthcare professionals employ various procedures, including a detailed medical history and physical examination, laboratory tests, and imaging tests.
Medical History and Physical Examination
A comprehensive medical history, including questions about current and past medical conditions, lifestyle factors, and exposure to environmental toxins, provides valuable insight into potential causes of azoospermia. A physical examination may also be conducted to identify any abnormalities in the reproductive system.
Laboratory Tests
Laboratory tests play a crucial role in diagnosing azoospermia. Semen analysis is typically the first step, where multiple semen samples are analyzed to confirm the absence of sperm. Hormone tests, genetic tests, and testicular biopsies may also be performed to identify underlying causes.
Imaging Tests
Imaging tests such as ultrasounds, magnetic resonance imaging (MRI), and computed tomography (CT) scans can help identify any structural abnormalities within the reproductive system that may be causing azoospermia. These tests provide valuable visual information for the healthcare team.
Treatment Options for Azoospermia
While azoospermia poses challenges to natural conception, various treatment options are available to increase the chances of fertility and parenthood.
Medication and Hormonal Therapy
In some cases, azoospermia may be treated with medication or hormonal therapy to address underlying hormonal imbalances or induce sperm production.
Surgical Procedures
Surgical procedures, such as sperm retrieval techniques (e.g., testicular sperm extraction or epididymal sperm aspiration), can be employed to collect viable sperm for use in assisted reproductive technologies (ART). These procedures aim to extract sperm directly from the testicles or epididymis and can be successful in cases of non-obstructive azoospermia.
Assisted Reproductive Technology
In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) are commonly utilized in cases of azoospermia. These ART techniques involve the fertilization of eggs with the retrieved sperm in a laboratory setting, followed by the transfer of embryos into the female partner’s uterus. Success rates vary depending on individual circumstances and the quality of retrieved sperm.
While the absence of sperm in the ejaculate presents challenges to natural conception, advancements in reproductive medicine and technology offer hope for individuals and couples looking to build a family. Seeking appropriate medical advice and emotional support can help navigate the complexities associated with azoospermia and strive towards achieving parenthood.




