Discover the fascinating connection between Clomid and testosterone in this insightful article.
The Relationship Between Clomid and Testosterone
In recent years, there has been growing interest in the relationship between Clomid and testosterone. This article aims to provide an overview of Clomid and its impact on testosterone levels. We will explore how Clomid works, the role of testosterone in the body, the potential benefits and risks of using Clomid as a testosterone booster, and alternative options available.
Understanding Clomid: An Overview
Before delving into the relationship between Clomid and testosterone, it is essential to understand what Clomid is. Clomid, also known by its generic name clomiphene citrate, is a medication commonly used to treat infertility in women. Interestingly, it can also be prescribed off-label to increase testosterone production in men.

Clomid belongs to a class of medications called selective estrogen receptor modulators (SERMs). SERMs are substances that selectively bind to estrogen receptors in the body, exerting different effects depending on the tissue. In the case of men, Clomid acts as an anti-estrogen by blocking the effects of estrogen on certain cells, primarily in the hypothalamus. By blocking estrogen’s actions on the hypothalamus, Clomid indirectly stimulates the production of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland.
Clomid’s primary mechanism of action involves the regulation of the hypothalamic-pituitary-testicular axis, which plays a crucial role in testosterone production. By increasing the secretion of LH and FSH, Clomid stimulates the testicles to produce more testosterone. This boost in testosterone levels can have various effects on the body, which we will explore in more detail.
It is important to note that while Clomid is effective in boosting testosterone levels in some men, it may not work for everyone. Factors such as individual hormone levels, underlying health conditions, and the cause of low testosterone can influence Clomid’s effectiveness. Therefore, it is crucial for individuals considering Clomid therapy for increasing testosterone to consult with a healthcare provider specialized in hormone management.
The Role of Testosterone in the Body
Before diving into the impact of Clomid on testosterone, let’s understand the importance of testosterone in the body.
The Importance of Testosterone
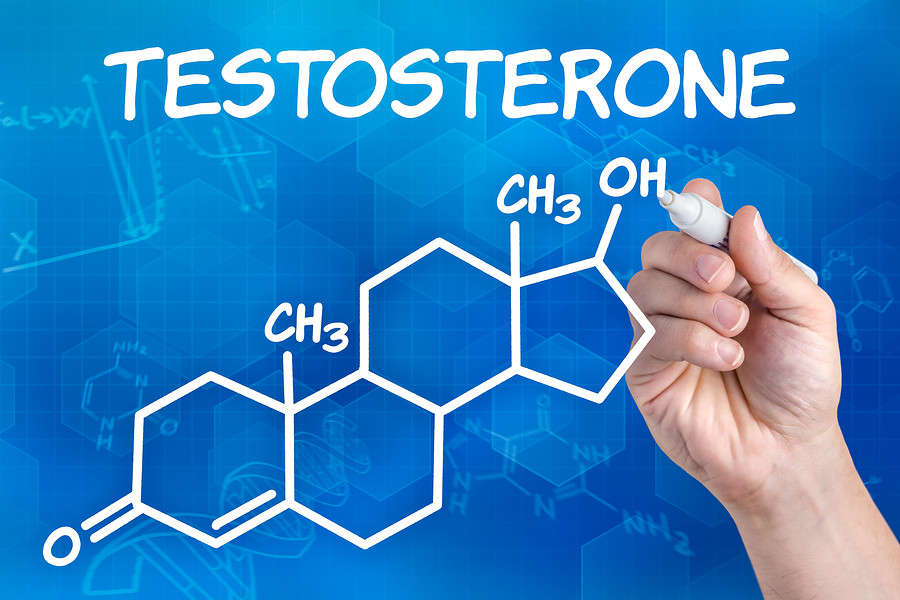
Testosterone is a hormone primarily produced in the testicles in men. It plays a significant role in various aspects of male health, including the development of secondary sexual characteristics, maintenance of muscle mass and bone density, regulation of mood, and sexual function. Testosterone also influences energy levels, cognitive function, and overall well-being.
In addition to its crucial role in male health, testosterone also has effects on women’s bodies, albeit in smaller amounts. Women produce testosterone in their ovaries and adrenal glands. It contributes to muscle strength, bone density, and libido in women. Maintaining a delicate balance of testosterone is essential for both men and women to support their overall health and well-being.
Factors Affecting Testosterone Levels
Testosterone levels can be influenced by various factors. Age, lifestyle choices, genetics, overall health, and underlying medical conditions can all impact testosterone production. It is essential to maintain optimal levels of testosterone to support general well-being and vitality.
Exercise and diet play a significant role in regulating testosterone levels. Regular physical activity, especially strength training, can help boost testosterone production. Additionally, a balanced diet rich in nutrients like zinc, vitamin D, and healthy fats is crucial for supporting healthy testosterone levels. Adequate sleep and stress management also play a vital role in maintaining optimal testosterone levels.
Clomid as a Testosterone Booster
Now that we have explored the basics of Clomid and testosterone, let’s delve deeper into the science behind Clomid as a testosterone booster.
The Science Behind Clomid and Testosterone
Studies have shown that Clomid can effectively increase testosterone levels in men with low testosterone or hypogonadism. By suppressing estrogen’s negative feedback on the hypothalamus, Clomid stimulates the production of LH and FSH, leading to enhanced testosterone production.
Furthermore, research suggests that Clomid may also have a positive impact on sperm production in men. This dual benefit of increasing testosterone levels and improving sperm quality makes Clomid a versatile option for men struggling with fertility issues.
It is worth noting that Clomid is not approved by regulatory agencies specifically for use as a testosterone booster. It is typically prescribed off-label and should only be used under medical supervision.
Potential Benefits of Using Clomid for Testosterone
The potential benefits of Clomid as a testosterone booster vary depending on individual factors, such as the underlying cause of low testosterone and overall health. Some potential benefits reported by users include increased libido, improved mood, enhanced muscle mass, increased energy levels, and improved cognitive function. However, it is important to note that results may vary, and Clomid may not be suitable for everyone.
Moreover, recent studies have suggested that Clomid may also have a role in preventing bone loss and improving bone mineral density in men with low testosterone levels. This additional benefit highlights the potential of Clomid as a multifaceted treatment option for men facing the challenges of low testosterone.
Risks and Side Effects of Clomid
As with any medication, Clomid carries risks and side effects that users should be aware of. It is important to understand the potential implications of using Clomid and to be informed about the various aspects of its effects on the body.
Clomid, also known as clomiphene citrate, is commonly prescribed to help stimulate ovulation in women struggling with infertility. However, its use is not without potential side effects and risks that users should consider before starting treatment.
Common Side Effects of Clomid
Common side effects of Clomid may include hot flashes, mood swings, nausea, headaches, visual disturbances, and changes in libido. These side effects can vary in intensity from mild to severe and may impact individuals differently. It is essential to discuss any side effects experienced while taking Clomid with a healthcare provider to determine the best course of action and ensure the well-being of the patient.
Long-Term Risks of Clomid Use
While Clomid is generally considered safe for short-term use in fertility treatments, the long-term risks of its use as a testosterone booster are not well-studied. Prolonged use of Clomid may have potential implications for cardiovascular health and fertility that users should be aware of. It is crucial for individuals considering extended Clomid use to weigh the benefits against the risks and to consult with a healthcare provider regularly to monitor any potential adverse effects.
Regular follow-up appointments with a healthcare provider are recommended for individuals using Clomid for an extended period to assess the ongoing impact of the medication on their health and well-being. Monitoring key health indicators and discussing any concerns or changes experienced during treatment can help ensure the safe and effective use of Clomid for its intended purpose.
Alternatives to Clomid for Boosting Testosterone
For those who may not be suitable candidates for Clomid or prefer alternative options, there are natural and pharmaceutical alternatives worth exploring.
When considering alternatives to Clomid for boosting testosterone, it’s essential to delve into the realm of natural remedies and pharmaceutical interventions. Understanding the various options available can empower individuals to make informed decisions about their health and well-being.
Natural Ways to Boost Testosterone

Several lifestyle factors can contribute to optimizing testosterone levels naturally. These include maintaining a healthy weight, regular exercise, stress management, quality sleep, balanced nutrition, and avoiding excessive alcohol consumption. Embracing a holistic approach to health by incorporating these practices can not only enhance testosterone levels but also improve overall quality of life.
Furthermore, exploring the world of herbal supplements like ashwagandha, tribulus terrestris, and fenugreek may offer additional support in naturally boosting testosterone levels. These herbs have been traditionally used for their potential benefits in enhancing male hormonal health, but it’s crucial to consult with a healthcare provider before integrating them into your routine.
Other Medications for Increasing Testosterone
In addition to Clomid, other medications, such as testosterone replacement therapy (TRT), may be prescribed to individuals with clinically low testosterone levels. TRT involves the administration of testosterone via injections, gels, patches, or pellets under medical supervision. This treatment option is tailored to each individual’s specific needs and monitored closely to ensure optimal results and safety.
Moreover, exploring the landscape of selective estrogen receptor modulators (SERMs) like tamoxifen as an alternative pharmaceutical approach to boosting testosterone levels can provide additional insights into personalized treatment plans. These medications work by blocking the effects of estrogen in the body, potentially leading to an increase in testosterone production.
Conclusion
In conclusion, Clomid can play a role in boosting testosterone levels in men with low testosterone. By acting as an anti-estrogen and stimulating LH and FSH production, Clomid indirectly enhances testosterone production. However, it is vital to understand the potential benefits and risks associated with Clomid use, as well as explore alternative options available. Always consult with a healthcare provider to determine the most appropriate approach for optimizing testosterone levels and overall well-being.





