Understanding Miscarriages: Causes, Symptoms, and Treatment Options

In recent years, the topic of miscarriages has increasingly garnered attention, leading to a deeper understanding of the complex factors that contribute to the loss of a pregnancy. This article delves into the multifaceted causes of miscarriages, which range from chromosomal abnormalities and maternal health conditions to lifestyle factors and environmental influences. Furthermore, we explore the available treatment options and preventative measures to help couples facing this emotionally devastating experience. By shedding light on this sensitive issue, we aim to foster informed conversations, promote awareness, and ultimately contribute to the development of more effective strategies for managing and preventing miscarriages.
Table of contents
Introduction to Miscarriages
A miscarriage is the involuntary loss of a pregnancy before the 20th week. Unfortunately, miscarriages are quite common, occurring in approximately 10% to 20% of known pregnancies. The majority of miscarriages occur during the first trimester, and most are due to natural causes. It’s essential to understand the different types of miscarriages, their causes, symptoms, and treatment options to help you navigate this challenging experience.
Types of Miscarriages
There are several types of miscarriages, each with its own set of characteristics:
- Threatened miscarriage: Vaginal bleeding occurs, but the cervix remains closed. The pregnancy may continue without complications.
- Inevitable miscarriage: Heavy bleeding, cramping, and an open cervix indicate that a miscarriage is imminent.
- Incomplete miscarriage: Some, but not all, of the pregnancy tissue has been expelled from the uterus.
- Complete miscarriage: All pregnancy tissue has been expelled from the uterus.
- Missed miscarriage: The embryo or fetus has stopped developing, but the body has not yet expelled the pregnancy tissue.
- Recurrent miscarriage: Three or more consecutive miscarriages.
Causes of Miscarriages
Miscarriages can be caused by various factors, including:
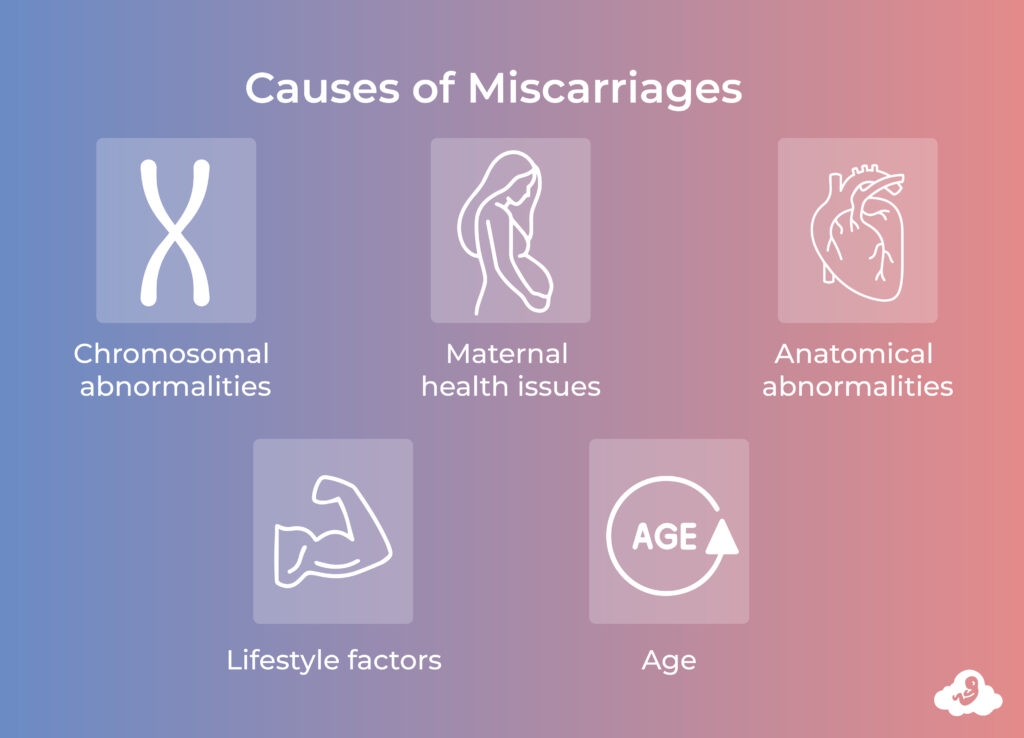
- Chromosomal abnormalities: Most early losses are due to chromosomal issues in the developing embryo or fetus, such as extra or missing chromosomes. These abnormalities typically occur by chance and are not inherited.
- Maternal health issues: Conditions like uncontrolled diabetes, infections, thyroid disorders, and autoimmune diseases can increase the risk of pregnancy loss.
- Anatomical abnormalities: Structural abnormalities in the uterus, such as fibroids or a septate uterus, can interfere with implantation or cause complications during pregnancy.
- Lifestyle factors: Smoking, alcohol consumption, and drug use can all contribute to the risk of early loss.
- Age: The risk of pregnancy loss increases with age, especially for women over 35.
Symptoms and Warning Signs
Some common symptoms and warning signs of a stillbirth include:
- Vaginal bleeding or spotting
- Cramping or pain in the abdomen or lower back
- Fluid or tissue passing from the vagina
- Loss of pregnancy symptoms, such as breast tenderness or nausea
If you experience any of these symptoms, contact your healthcare provider immediately, preferably an OB/GYN or REI doctors.
Diagnosis and Tests
To diagnose a miscarriage, your healthcare provider may perform the following tests:
- Physical examination: Assessing your symptoms and checking the cervix for dilation.
- Blood tests: Measuring hormone levels, such as human chorionic gonadotropin (hCG), to determine the viability of the pregnancy.
- Ultrasound: Visualizing the embryo or fetus and checking for a heartbeat.
- Tissue tests: Analyzing expelled tissue to determine the cause of the pregnancy loss, especially in cases of multiple recurrences.
Treatment and Recovery
The appropriate treatment for a miscarriage depends on the type and severity of the situation:
- Expectant management: In some cases, your healthcare provider may recommend waiting for the miscarriage to progress naturally. This approach is typically used for early losses or when the pregnancy tissue is expected to pass without intervention.
- Medical management: Medications may be prescribed to help the body expel the pregnancy tissue. This is usually done in cases of incomplete or missed miscarriages.
- Surgical management: A procedure called dilation and curettage (D&C) may be performed to remove the pregnancy tissue from the uterus, particularly in cases of incomplete or missed miscarriages where other treatments are ineffective or not recommended.
After an early loss, it’s essential to allow yourself time to heal, both physically and emotionally. Follow your healthcare provider’s recommendations for recovery, which may include getting plenty of rest, avoiding strenuous activities, and waiting a certain period before trying to conceive again.
Preventing Miscarriages
While many miscarriages are due to factors beyond your control, there are some steps you can take to reduce your risk:
- Maintain a healthy lifestyle: Eat a balanced diet, exercise regularly, get enough sleep, and manage stress.
- Avoid harmful substances: Refrain from smoking, drug use, and limit alcohol consumption.
- Manage pre-existing conditions: Keep chronic health issues, such as diabetes or thyroid disorders, under control.
- Take prenatal vitamins: Begin taking prenatal vitamins before trying to conceive to ensure you’re getting essential nutrients like folic acid.
- Seek early prenatal care: Regular check-ups with your healthcare provider can help detect and manage any potential complications.
Coping with Loss
Experiencing a miscarriage can be an emotionally challenging event. It’s essential to allow yourself time to grieve and seek support from friends, family, or a mental health professional if needed. Joining a support group, talking to others who had a similar experience, or exploring therapy options can provide valuable assistance during this difficult time.
Remember that it’s common for women who have went through losses to go on to have successful pregnancies in the future. Don’t lose hope, and give yourself the time and space to heal physically and emotionally before trying to conceive again.