Discover how poor gut health may increase inflammation and immune responses that threaten early pregnancy.
Understanding Gut Health and Its Systemic Effects
The human gut is home to a complex ecosystem of microorganisms collectively known as the gut microbiome. This intricate community plays a vital role not only in digestion but also in regulating the immune system. Recent research has increasingly highlighted the gut’s influence beyond the digestive tract, affecting systemic inflammation and immune responses that can have far-reaching consequences.

Gut health refers to the balance and function of this microbiome, the integrity of the intestinal lining, and the gut’s ability to communicate with other bodily systems. When gut health is compromised, it can lead to dysbiosis, an imbalance in microbial populations. This imbalance is often linked to increased intestinal permeability, sometimes called “leaky gut,”. This allows toxins and bacteria to enter the bloodstream and trigger systemic inflammation.
The Gut Microbiome: Composition and Function
The gut microbiome consists of trillions of bacteria, viruses, fungi, and other microorganisms. These microbes perform essential functions, including fermenting dietary fibers to produce short-chain fatty acids (SCFAs) like butyrate. This nourishes intestinal cells and modulate inflammation. The diversity and composition of the microbiome vary widely among individuals, influenced by genetics, diet, environment, and lifestyle.
Beneficial bacteria such as Lactobacillus and Bifidobacterium species help maintain a balanced immune response and protect against pathogenic microbes. Conversely, an overgrowth of harmful bacteria or a reduction in beneficial species can disrupt gut homeostasis. This disruption may contribute to chronic low-grade inflammation. This is which is increasingly recognized as a factor in various diseases, including metabolic disorders, autoimmune conditions, and reproductive challenges. The gut microbiome plays a role in synthesizing essential vitamins and nutrients, such as vitamin K and certain B vitamins. These are crucial for maintaining energy levels and overall vitality.
How Gut Health Influences Inflammation Throughout the Body
The gut microbiome communicates with the immune system through multiple pathways. Gut-associated lymphoid tissue (GALT) represents a significant portion of the body’s immune cells, and the microbiome helps educate and regulate these immune responses. When gut barrier integrity is compromised, bacterial components such as lipopolysaccharides (LPS) can translocate into the bloodstream, activating systemic inflammatory pathways.
This systemic inflammation is characterized by elevated levels of pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). Chronic inflammation can disrupt normal physiological processes and has been linked to complications in various organ systems. Inflammation plays a critical role in reproductive health. This is particularly during early pregnancy. This is where immune tolerance and controlled inflammation are essential for successful implantation and fetal development. Emerging studies suggest that the gut-brain axis, a bidirectional communication system between the gut and the central nervous system. This may also be influenced by gut health. This connection implies that imbalances in the gut microbiome could potentially affect mental health outcomes. This leads to conditions such as anxiety and depression. This thereby underscores the importance of maintaining a healthy gut for both physical and mental well-being.
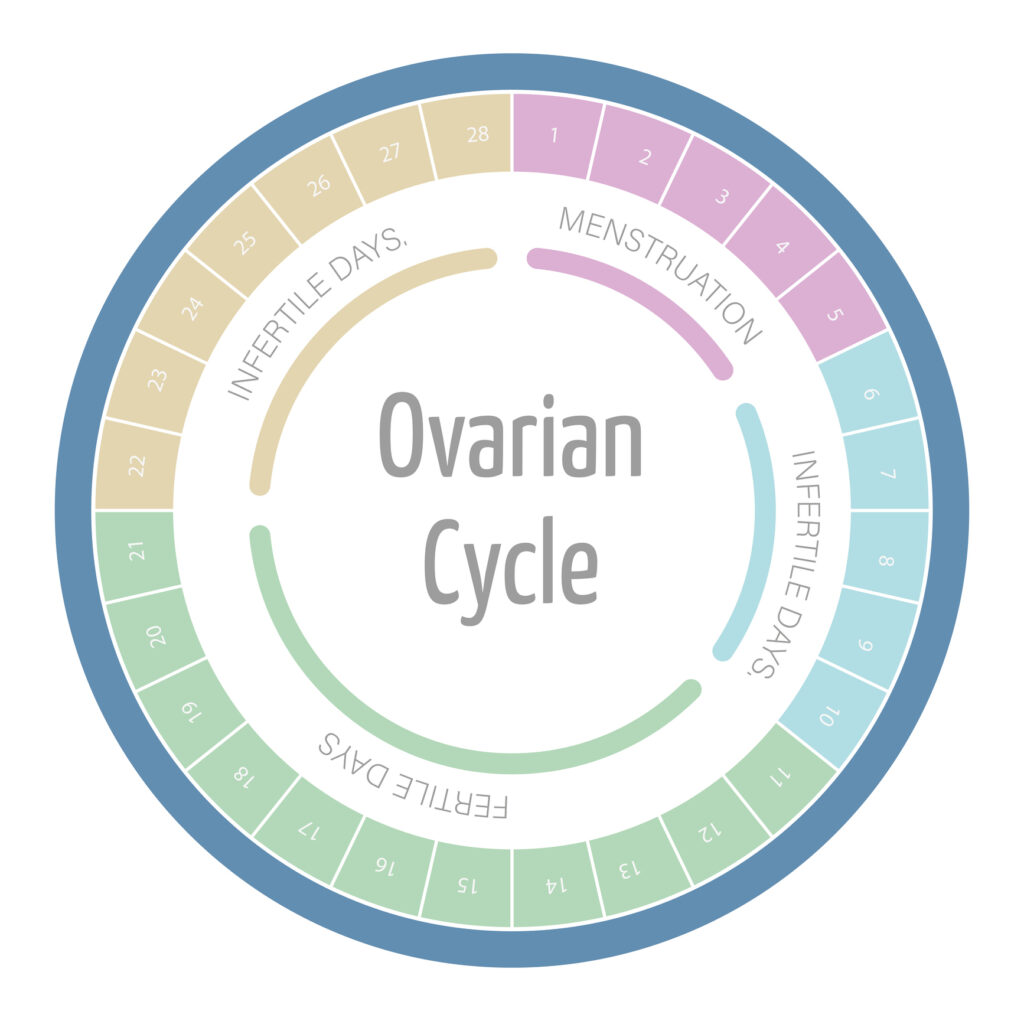
The Connection Between Gut Health and Pregnancy
Pregnancy is a unique immunological state requiring a delicate balance between immune activation and tolerance. The maternal immune system must accept the semi-allogenic fetus while still protecting against infections. Emerging evidence suggests that gut health and the microbiome are integral to this balance, influencing inflammatory and immune responses during early pregnancy. The gut microbiome, a complex community of microorganisms residing in the digestive tract, plays a pivotal role in shaping the immune system and can significantly impact maternal and fetal health.
Disruptions in gut microbiota composition and increased intestinal permeability may contribute to heightened systemic inflammation, potentially affecting pregnancy outcomes. For instance, conditions such as dysbiosis, characterized by an imbalance of beneficial and harmful gut bacteria, have been linked to various pregnancy complications, including gestational diabetes and hypertensive disorders. Understanding this connection is crucial for identifying modifiable factors that can support reproductive health and reduce the risk of pregnancy complications. Dietary interventions, such as increasing fiber intake and consuming probiotics, may help restore a healthy microbiome, thereby promoting better pregnancy outcomes.
Inflammatory Markers and Their Impact on Implantation
Successful implantation of the embryo into the uterine lining is a highly regulated process involving immune cells and inflammatory mediators. While a certain degree of localized inflammation is necessary to facilitate implantation, excessive or systemic inflammation can be detrimental. Elevated inflammatory markers such as C-reactive protein (CRP), TNF-α, and IL-6 have been associated with implantation failure and early pregnancy loss. These markers can serve as indicators of the body’s inflammatory status and may provide insight into the underlying mechanisms affecting implantation.
Studies have shown that women with poor gut health often exhibit higher circulating levels of these pro-inflammatory cytokines. This suggests that gut-derived inflammation may interfere with the uterine environment, impairing embryo implantation. Moreover, systemic inflammation can alter hormone signaling and vascular function, further complicating early pregnancy success. Research indicates that optimizing gut health through dietary modifications, such as incorporating fermented foods rich in probiotics, may help lower these inflammatory markers, thereby enhancing the likelihood of successful implantation and a healthy pregnancy.
Immune System Regulation During Early Pregnancy
During early pregnancy, the immune system undergoes significant modulation to promote fetal tolerance. Regulatory T cells (Tregs) increase in number to suppress potentially harmful immune responses against the fetus. The gut microbiome influences the development and function of these immune cells through the production of metabolites like SCFAs, which have anti-inflammatory properties. These metabolites not only contribute to immune regulation but also support the integrity of the gut barrier, further emphasizing the interconnectedness of gut health and immune function.
Disruption of the gut microbiota can impair Treg function and skew the immune balance toward a pro-inflammatory state. This dysregulation may increase the risk of pregnancy complications such as miscarriage, preeclampsia, and preterm birth. Furthermore, the maternal diet during pregnancy can significantly influence the gut microbiome composition, highlighting the importance of nutritional choices. Consuming a diverse array of whole foods, particularly those high in fiber, can foster a robust and balanced microbiome, ultimately supporting the immune adaptations necessary for a healthy pregnancy. As research continues to uncover the complexities of the gut-microbiome-pregnancy relationship, it becomes increasingly clear that nurturing gut health is a vital aspect of prenatal care.
Strategies to Improve Gut Health for Pregnancy Success
Given the growing understanding of gut health’s role in inflammation and immune regulation during pregnancy, adopting strategies to support the gut microbiome is an important consideration for women planning to conceive or in early pregnancy. These strategies focus on dietary modifications, lifestyle changes, and targeted supplementation to restore microbial balance and reduce inflammation.

Dietary Approaches to Reduce Inflammation and Support Gut Health
A nutrient-rich, anti-inflammatory diet is foundational for promoting gut health. Emphasizing whole foods such as fruits, vegetables, whole grains, nuts, and seeds provides dietary fiber that feeds beneficial gut bacteria and encourages SCFA production. The Mediterranean diet, rich in omega-3 fatty acids, antioxidants, and polyphenols, has been shown to reduce systemic inflammation and improve microbial diversity.
Conversely, diets high in processed foods, refined sugars, and saturated fats can promote dysbiosis and inflammation. Limiting these foods while ensuring adequate intake of vitamins and minerals—particularly folate, vitamin D, and iron, which are critical during pregnancy—supports both gut and reproductive health. Hydration and regular physical activity also contribute positively to gut motility and microbiome composition. Additionally, incorporating fermented foods like yogurt, kefir, sauerkraut, and kimchi can introduce beneficial probiotics directly into the diet, further enhancing gut health and supporting the immune system.
Probiotic and Prebiotic Interventions for Reproductive Health
Probiotics are live microorganisms that, when administered in adequate amounts, confer health benefits to the host. Certain probiotic strains, including Lactobacillus rhamnosus and Bifidobacterium lactis, have demonstrated potential in modulating immune responses and reducing inflammation. Clinical trials suggest that probiotic supplementation may improve pregnancy outcomes by enhancing gut barrier function and promoting a balanced immune environment.
Prebiotics, non-digestible fibers that stimulate the growth of beneficial bacteria, also play a critical role. Foods rich in prebiotics include garlic, onions, asparagus, and bananas. Combining probiotics with prebiotics (synbiotics) may offer synergistic benefits. However, it is important for women to consult healthcare providers before starting supplements, especially during pregnancy, to ensure safety and appropriateness. Furthermore, emerging research indicates that the timing of probiotic and prebiotic intake can influence their effectiveness, suggesting that early intervention may be particularly beneficial for women trying to conceive or those in the early stages of pregnancy.
In conclusion, poor gut health can increase systemic inflammation and alter immune responses, potentially harming early pregnancy. Understanding and supporting gut health through diet, lifestyle, and targeted interventions may improve reproductive outcomes and promote a healthy pregnancy journey.
References:
- National Institute of Diabetes and Digestive and Kidney Diseases. (2023). Gut Microbiome.
- Centers for Disease Control and Prevention. (2022). Pregnancy and Maternal Health.
- American Journal of Reproductive Immunology. (2021). The Role of Inflammation in Early Pregnancy and Implantation.
- World Health Organization. (2023). Preterm Birth Fact Sheet.
- Harvard T.H. Chan School of Public Health. (2023). Diet and Inflammation.