“Uncover the reasons behind spotting before your period and learn when it’s normal and when to be concerned.
Spotting before a period can be concerning for many women, and understanding the causes behind it is essential for proper management and peace of mind. In this article, we will delve into the intricacies of the menstrual cycle, define spotting, explore its causes, and address when it’s necessary to be concerned.
Understanding the Menstrual Cycle
Normal Menstrual Cycle
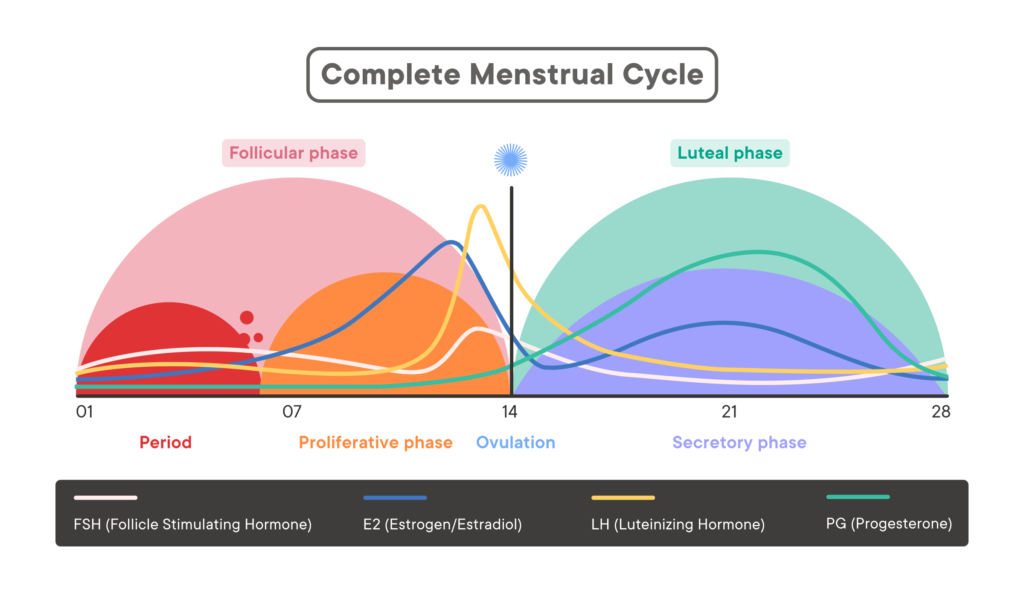
The menstrual cycle is a complex process that involves hormonal changes and the shedding of the uterine lining. On average, a typical menstrual cycle lasts 28 days, with slight variations considered normal. It is divided into two phases: the follicular phase and the luteal phase.
During the follicular phase, which lasts approximately 14 days, the pituitary gland releases follicle-stimulating hormone (FSH), stimulating the development of an egg in the ovaries. Simultaneously, estrogen levels rise, thickening the uterine lining in preparation for potential pregnancy.
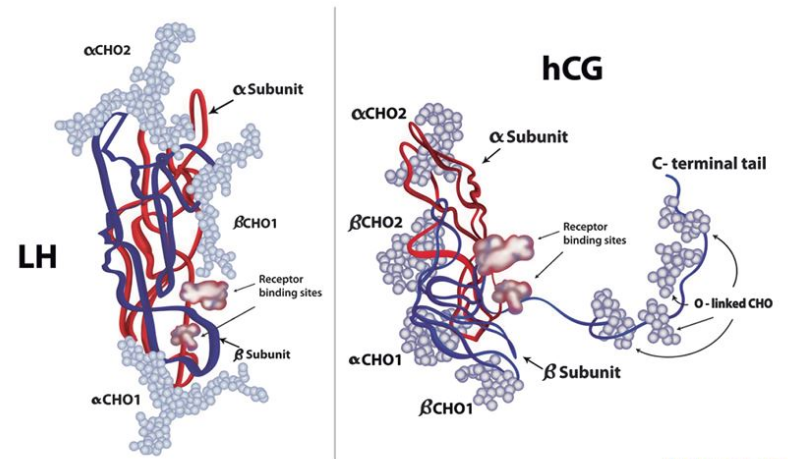
Following the follicular phase, ovulation occurs when the mature egg is released from the ovary. This signals the transition to the luteal phase, which lasts around 14 days. During this phase, the pituitary gland produces luteinizing hormone (LH), triggering the production of progesterone. Progesterone helps maintain the thickened uterine lining and prepares the body for pregnancy.
If fertilization does not occur, hormone levels drop, leading to the shedding of the uterine lining and the onset of menstruation.
Variations in the Menstrual Cycle
While a 28-day cycle is considered average, it is important to note that variations are common and normal. Some women may have shorter cycles of around 21 days, while others may experience longer cycles of 35 days or more. Additionally, variations in the length and intensity of menstruation can occur from month to month.
Factors such as stress, lifestyle changes, and certain medical conditions can influence the length and regularity of the menstrual cycle. It is crucial to be aware of your own unique cycle patterns to identify any abnormal changes that may warrant further investigation.
Furthermore, it is worth mentioning that the menstrual cycle is not just about the physical changes that occur in the body. It is also influenced by a complex interplay of emotions and psychological factors. Many women experience mood swings, irritability, and even depression during certain phases of their cycle. This is believed to be due to the fluctuating levels of hormones, particularly estrogen and progesterone, which can affect neurotransmitters in the brain.
Moreover, the menstrual cycle is not limited to its reproductive function. It also plays a role in maintaining overall health. For example, estrogen, one of the key hormones involved in the menstrual cycle, helps regulate bone density. This is why women are at a higher risk of developing osteoporosis after menopause, when estrogen levels decline.
Defining Spotting
Spotting vs Regular Menstruation
Spotting refers to the light discharge of blood from the vagina that may occur between periods. It is often characterized by its minimal flow and shorter duration compared to a regular menstrual period. While spotting can be normal for some women, especially during ovulation or in the days leading up to menstruation, it can also indicate underlying health issues.

Understanding the difference between spotting and regular menstruation is crucial for women’s reproductive health. While spotting may be light and intermittent, a regular menstrual period typically involves a more consistent flow of blood over several days. It’s essential to track your menstrual cycle to identify any irregularities that may signal potential health concerns.
Frequency and Duration of Spotting
The frequency and duration of spotting episodes can vary from woman to woman. Some may experience occasional spotting that lasts only a day or two, while others may have more frequent episodes that persist for several days or even weeks.
Factors such as hormonal fluctuations, stress, changes in birth control methods, or underlying medical conditions can influence the frequency and duration of spotting. Keeping a menstrual diary can help you monitor these patterns and provide valuable information to your healthcare provider.
If you notice an increase in the frequency or duration of spotting, it is essential to pay attention to other accompanying symptoms and seek medical advice if necessary.
Causes of Spotting Before Period
Hormonal Changes
Hormonal fluctuations throughout the menstrual cycle can be a common cause of spotting before a period. These changes can disrupt the regularity of the menstrual cycle, leading to spotting in some cases.
One possible cause of hormonal imbalance is polycystic ovary syndrome (PCOS), a common hormonal disorder among women of reproductive age. PCOS can result in irregular periods, including spotting between cycles.
Other factors, such as thyroid disorders or certain medications, can also impact hormone levels and contribute to spotting.
Contraceptive Use
Spotting can also be a side effect of hormonal contraceptives, such as birth control pills, patches, or intrauterine devices (IUDs). These contraceptive methods often contain hormones that regulate the menstrual cycle, but they can occasionally cause breakthrough bleeding or spotting.
If you are experiencing spotting while using hormonal contraceptives, consulting with your healthcare provider can help determine if a different contraceptive method or adjustment in dosage is necessary.
Pregnancy and Miscarriage
While implantation bleeding can sometimes be mistaken for spotting before a period, it is important to be aware that pregnancy can cause light bleeding or spotting in the early stages. If you suspect you may be pregnant and are experiencing spotting, consider taking a pregnancy test and consult with your healthcare provider for further guidance.
In some unfortunate cases, spotting before a period can also be a sign of a miscarriage. If you have had a positive pregnancy test and are experiencing spotting accompanied by severe cramping or tissue passing, it is crucial to seek immediate medical attention.
Gynecological Conditions
Various gynecological conditions can contribute to spotting before a period. Conditions such as endometriosis, uterine fibroids, and cervical or uterine polyps can cause irregular bleeding and spotting throughout the menstrual cycle.
If you have a known gynecological condition and are experiencing unusual spotting, it is important to keep your healthcare provider informed to ensure proper monitoring and management of your condition.
Understanding the causes of spotting before a period can provide valuable insight into your reproductive health. By recognizing the potential underlying factors, you can take proactive steps to address any concerns and seek appropriate medical guidance.
It is worth noting that stress and lifestyle factors can also influence the regularity of your menstrual cycle and potentially contribute to spotting. Engaging in stress-reducing activities, maintaining a balanced diet, and practicing regular exercise can help support overall reproductive health.
When to Be Concerned About Spotting
Persistent Spotting
If you have persistent spotting that occurs outside of your regular menstrual cycle or exceeds what is considered normal for you, it is important to consider it warranting further investigation. Persistent spotting can indicate underlying health issues that require medical attention.
One possible cause of persistent spotting is hormonal imbalance. This can occur due to various factors such as stress, changes in weight, or certain medical conditions. It is important to consult with your healthcare provider to determine the underlying cause and appropriate treatment.
Accompanying Symptoms
While spotting alone may not always be a cause for alarm, the presence of certain accompanying symptoms should raise concerns. Symptoms such as severe pelvic pain, foul-smelling discharge, or fever warrant immediate medical attention as they may indicate an infection or other serious condition.
In addition to these symptoms, it is also important to pay attention to the color and consistency of the spotting. Bright red blood may indicate fresh bleeding, while dark brown or black blood may suggest older blood. Your healthcare provider will take all of these factors into consideration when evaluating your condition.
Spotting and Age Factors
For women approaching menopause, spotting before a period can be part of the natural hormonal transition. However, if you are under the age of 40 and are experiencing irregular or prolonged spotting, it is advisable to consult with your healthcare provider to rule out any potential underlying conditions.
There are various factors that can contribute to irregular spotting in younger women, such as polycystic ovary syndrome (PCOS), uterine fibroids, or thyroid disorders. Your healthcare provider will be able to conduct the necessary tests and examinations to determine the cause of your spotting and provide appropriate treatment options.
By understanding the causes and concerns surrounding spotting before a period, women can have greater insight into their own menstrual health. Regular communication with healthcare providers and being proactive about understanding one’s own body is crucial in ensuring optimal reproductive health.