Uncover the intricate link between elevated estradiol levels and PCOS in this comprehensive article.
What is the connection between high estradiol and PCOS?
Polycystic Ovary Syndrome (PCOS) is a complex hormonal condition that affects millions of women worldwide. While the exact cause of PCOS remains unknown, researchers have identified several factors that contribute to its development and progression. One such factor is high levels of estradiol, a form of estrogen that plays a crucial role in the female reproductive system. In this article, we will explore the connection between high estradiol and PCOS, examining the functions of estradiol, the symptoms and impact of PCOS, hormonal imbalances, potential treatments, and the future of research in this field.
Understanding Estradiol and Its Functions

Estradiol is the most active and potent form of estrogen in the female body. It is primarily produced by the ovaries, but small amounts are also synthesized in other tissues, such as adipose (fat) cells. Estrogen, including estradiol, plays a vital role in regulating the menstrual cycle, supporting reproductive health, and maintaining bone density. Additionally, it influences mood, cognitive function, and cardiovascular health.
The Role of Estradiol in the Female Body
Estradiol is responsible for the development and maturation of the female reproductive system. During puberty, it stimulates the growth of breasts, pubic hair, and the widening of the hips. Throughout the menstrual cycle, estradiol levels fluctuate, contributing to the development and release of a mature egg from the ovaries. It also promotes the thickening of the uterine lining to prepare for pregnancy. In menopause, when estrogen production declines significantly, estradiol levels diminish, leading to various symptoms such as hot flashes and vaginal dryness.
How Estradiol Levels are Regulated
Estradiol levels are regulated by a complex interplay of hormones, including follicle-stimulating hormone (FSH) and luteinizing hormone (LH), both produced by the pituitary gland in the brain. FSH stimulates the growth of follicles in the ovaries, which contain the eggs. As the follicles develop, they produce estradiol, which signals the pituitary gland to decrease the production of FSH and increase the production of LH. Eventually, a surge of LH triggers ovulation. After ovulation, the ruptured follicle transforms into the corpus luteum, a temporary endocrine gland that produces progesterone and additional estradiol.
It is fascinating to note that estradiol not only affects the reproductive system but also has a significant impact on mood and cognitive function. Research has shown that estradiol has neuroprotective effects, meaning it helps to preserve and protect brain cells. It has been linked to improved memory, attention, and overall cognitive performance. This is why fluctuations in estradiol levels during the menstrual cycle can sometimes lead to changes in mood and cognitive abilities.
Furthermore, estradiol plays a crucial role in cardiovascular health. It helps to maintain the elasticity of blood vessels, promoting healthy blood flow and reducing the risk of cardiovascular diseases. Studies have shown that estradiol can have a positive effect on cholesterol levels, increasing the levels of “good” cholesterol (HDL) and decreasing the levels of “bad” cholesterol (LDL). This cholesterol-balancing effect helps to protect against the development of atherosclerosis, a condition characterized by the buildup of plaque in the arteries.
Polycystic Ovary Syndrome (PCOS) Explained
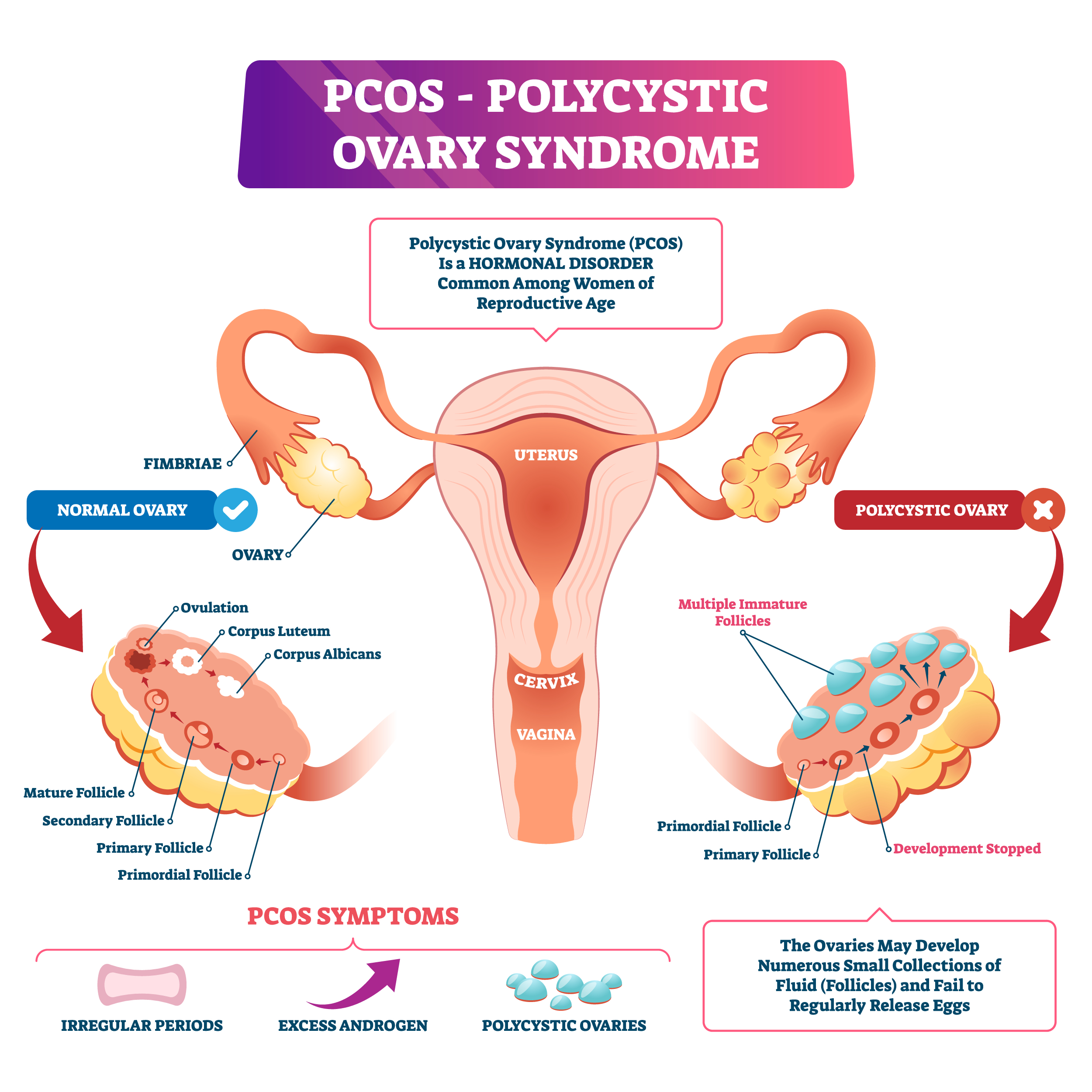
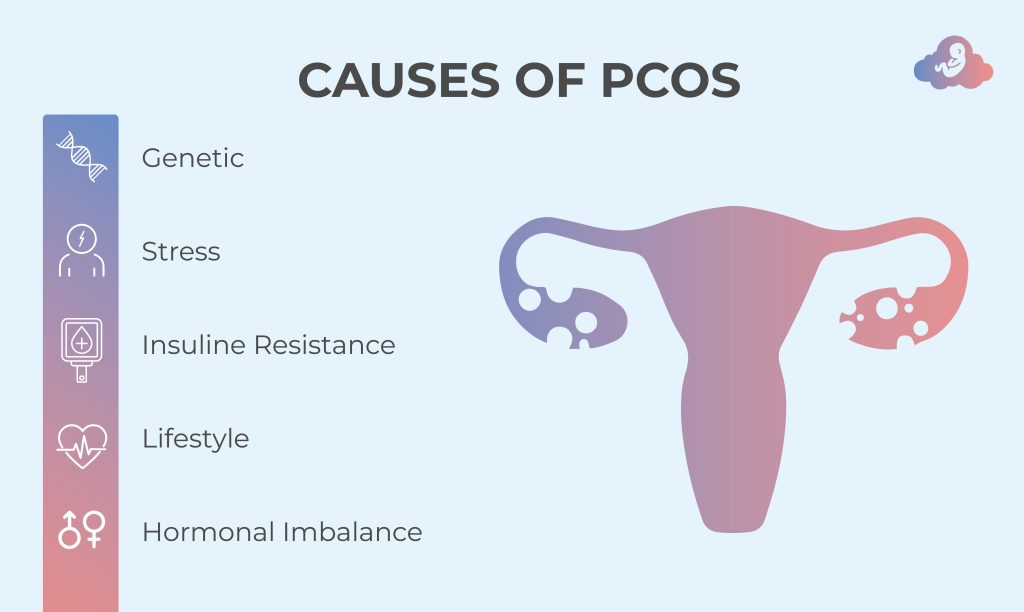
Polycystic Ovary Syndrome (PCOS) is a complex condition that affects the ovaries and hormonal balance in women. It is characterized by three main features: irregular or absent menstrual periods, excess androgen levels (male hormones), and the presence of multiple cysts on the ovaries. The exact cause of PCOS is still not fully understood, but both genetic and environmental factors are believed to play a role in its development.
Symptoms and Diagnosis of PCOS
The symptoms of PCOS vary from woman to woman. Some common signs include irregular menstrual cycles, heavy or prolonged periods, acne, excessive hair growth (hirsutism), and difficulty losing weight. These symptoms can be distressing and impact a woman’s quality of life. Women with PCOS may also experience infertility, insulin resistance, and an increased risk of developing type 2 diabetes and cardiovascular disease.
Diagnosis of PCOS involves evaluating symptoms, conducting hormonal tests to measure estradiol, FSH, LH, and androgen levels, and performing an ultrasound to examine the ovaries. It is important for healthcare providers to accurately diagnose PCOS in order to provide appropriate treatment and support.
The Impact of PCOS on Women’s Health
PCOS can significantly impact a woman’s physical and emotional well-being. The hormonal imbalances in PCOS can lead to weight gain, insulin resistance, and an increased risk of metabolic disorders. This can make it challenging for women with PCOS to maintain a healthy weight and manage their overall health.
Furthermore, women with PCOS may also experience psychological effects such as anxiety, depression, and poor self-image due to the visible symptoms associated with the condition. The presence of acne, excessive hair growth, and weight gain can affect a woman’s self-esteem and body image, leading to emotional distress.
Additionally, PCOS can pose challenges in conceiving naturally, requiring medical interventions such as fertility treatments. Many women with PCOS struggle with infertility, which can be emotionally and mentally draining. Seeking support from healthcare professionals and joining support groups can provide valuable resources and guidance for women navigating the complexities of PCOS.
The Link Between High Estradiol and PCOS
Hormonal imbalances, such as high levels of estradiol, are a hallmark of PCOS. In women with PCOS, the normal hormonal feedback loop that regulates the production and release of estradiol gets disrupted. This disruption can lead to an overproduction of estradiol, contributing to the development of cysts on the ovaries and interfering with normal ovulation. As a result, the menstrual cycle becomes irregular, and fertility may be compromised.
Furthermore, the impact of high estradiol levels on PCOS goes beyond reproductive health. Research suggests that elevated estradiol levels in women with PCOS may also be linked to an increased risk of cardiovascular disease. The intricate relationship between hormonal imbalances and long-term health outcomes underscores the importance of early detection and management of PCOS.
Hormonal Imbalances in PCOS
In addition to elevated estradiol levels, women with PCOS often have higher than normal levels of androgens, such as testosterone. This excess androgen production can further disrupt the hormonal balance, leading to the characteristic symptoms of PCOS. The hormonal imbalances associated with PCOS not only affect reproductive health but also impact metabolism, insulin sensitivity, and lipid levels in the bloodstream.
Moreover, the dysregulation of hormones in PCOS can manifest in various ways, including hirsutism (excessive hair growth), acne, and male-pattern baldness. These physical manifestations of hormonal imbalances can have significant psychological and emotional effects on individuals with PCOS, highlighting the need for a holistic approach to managing the condition.
Estradiol’s Impact on PCOS Development
While elevated estradiol levels are associated with PCOS, it is essential to understand that not all women with PCOS have high estradiol levels. The interplay between multiple hormones, including FSH, LH, and androgens, contributes to the development and progression of PCOS. However, high estradiol levels can exacerbate the symptoms and complications of PCOS, making it challenging to manage the condition effectively.
Furthermore, the role of estradiol in PCOS development extends beyond its effects on the reproductive system. Studies have shown that estradiol may also influence inflammatory pathways and insulin signaling, further complicating the metabolic aspects of PCOS. Understanding the multifaceted impact of estradiol on PCOS pathophysiology is crucial for developing targeted treatment strategies that address the underlying hormonal imbalances.
Potential Treatments for High Estradiol and PCOS
Managing high estradiol levels and PCOS requires a multifaceted approach that addresses hormonal imbalances, insulin resistance, and associated symptoms. The treatment plan may vary depending on individual needs and goals, but it generally includes lifestyle changes, natural remedies, and medical interventions.
When it comes to lifestyle changes, adopting a healthy and balanced routine can have a significant impact on estradiol levels and PCOS symptoms. Regular exercise, such as aerobic activities and strength training, not only helps with weight management but also improves insulin sensitivity. Engaging in physical activities like yoga or Pilates can aid in stress reduction, which is crucial for hormonal regulation. Additionally, incorporating a diet rich in nutrients, such as whole grains, lean proteins, and colorful fruits and vegetables, can provide the necessary building blocks for hormone production and overall well-being.
While lifestyle changes are essential, some individuals may find additional relief from PCOS symptoms through natural remedies. Herbal supplements, such as chasteberry and saw palmetto, have been traditionally used to support hormonal balance and reduce symptoms like irregular periods and acne. Acupuncture, an ancient practice rooted in traditional Chinese medicine, may also help regulate menstrual cycles and alleviate some of the discomfort associated with PCOS. However, it is crucial to consult with a healthcare professional before trying any natural remedies, as they may interact with other medications or have unintended side effects.
In more severe cases of PCOS, medical interventions may be necessary to manage high estradiol levels and mitigate the impact of the condition. Birth control pills, such as combination pills or progestin-only pills, are commonly prescribed to regulate menstrual cycles and reduce androgen production. Hormonal medications, such as anti-androgens or insulin-sensitizing drugs like metformin, can also be prescribed to improve insulin sensitivity and further regulate hormone levels. These medications work by targeting specific aspects of PCOS, helping to restore hormonal balance and alleviate symptoms.
For women struggling with infertility due to PCOS, fertility treatments may be recommended. Ovulation induction, which involves the use of medications to stimulate egg production, can increase the chances of successful conception. In more complex cases, in vitro fertilization (IVF) may be considered, where eggs are fertilized outside the body and then implanted into the uterus. These fertility treatments offer hope to individuals who desire to start or expand their families despite the challenges posed by PCOS.
The Future of Research in Estradiol and PCOS
As our understanding of PCOS and the role of estradiol continues to evolve, ongoing research is striving to uncover new treatment strategies and improve outcomes for women with PCOS.
Current Studies and Their Implications
Research is currently focusing on various aspects of PCOS, including the underlying genetic mechanisms, long-term health risks, and personalized treatment approaches. Studies are also investigating the potential role of new medications, such as selective estrogen receptor modulators (SERMs), in managing PCOS symptoms and hormonal imbalances.
Potential Breakthroughs in PCOS Treatment
As our knowledge of PCOS deepens, researchers aim to develop more targeted and effective treatments. Potential breakthroughs include the use of novel hormone-regulating medications, non-invasive diagnostic methods, and personalized treatment plans based on an individual’s unique hormonal profile. Additionally, advances in assisted reproductive technologies may provide new options for women with PCOS struggling with infertility.
In conclusion, high estradiol levels play a role in the development and complications of PCOS. While the precise connection between high estradiol and PCOS is complex and multifactorial, addressing hormonal imbalances and managing associated symptoms is crucial in effectively managing the condition. With ongoing research and advancements in treatment strategies, the future holds promise for improved outcomes and better quality of life for women affected by high estradiol and PCOS.