Discover how excessive screen time at night may disrupt melatonin and reproductive hormones.
The Science of Melatonin and Blue Light
How screens emit blue light and affect circadian rhythms
In today’s digital age, screens have become an integral part of daily life. Smartphones, tablets, laptops, and televisions all emit a specific type of light known as blue light. This high-energy visible (HEV) light is characterized by wavelengths between approximately 400 and 490 nanometers. It is especially potent at influencing our biological clocks.

Blue light exposure during the day can be beneficial, helping to boost alertness and cognitive function. When exposure occurs at night, it can disrupt the body’s natural circadian rhythms. This is the internal 24-hour cycles that regulate sleep-wake patterns and many physiological processes. The circadian rhythm is primarily governed by the suprachiasmatic nucleus (SCN) in the brain. This responds to light cues to synchronize bodily functions with the external environment. This synchronization is vital for maintaining not only sleep patterns but also hormonal balance, metabolism, and even mood regulation. This highlights the importance of managing light exposure throughout the day.
The physiological pathway from light exposure to melatonin suppression
Melatonin is produced by the pineal gland. It plays a crucial role in signaling the body that it is time to sleep. Its production typically begins in the evening as natural light fades, reaching peak levels during the night. Blue light exposure from screens can inhibit melatonin synthesis by stimulating specialized retinal cells called intrinsically photosensitive retinal ganglion cells (ipRGCs). These cells send signals to the SCN, which then suppresses melatonin production.
This suppression can delay the onset of sleep, reduce overall sleep quality, and shift circadian rhythms. According to the National Institute of General Medical Sciences, even short-term exposure to blue light at night can reduce melatonin levels by up to 50%, leading to difficulties in falling asleep and maintaining restorative sleep cycles. Chronic exposure to blue light at night has been linked to a range of health issues. This includes increased risk of obesity, diabetes, and cardiovascular diseases, as the disruption of sleep can lead to metabolic dysregulation. Understanding the intricate relationship between light exposure and melatonin production underscores the importance of mindful screen usage.
Connecting Melatonin Disruption to Reproductive Health
The relationship between melatonin and sex hormone production
While melatonin is widely recognized for its role in sleep regulation, it also influences reproductive hormones and fertility. Melatonin acts as an antioxidant and regulator within the reproductive system. They impact the secretion of hormones such as luteinizing hormone (LH), follicle-stimulating hormone (FSH), estrogen, and testosterone.
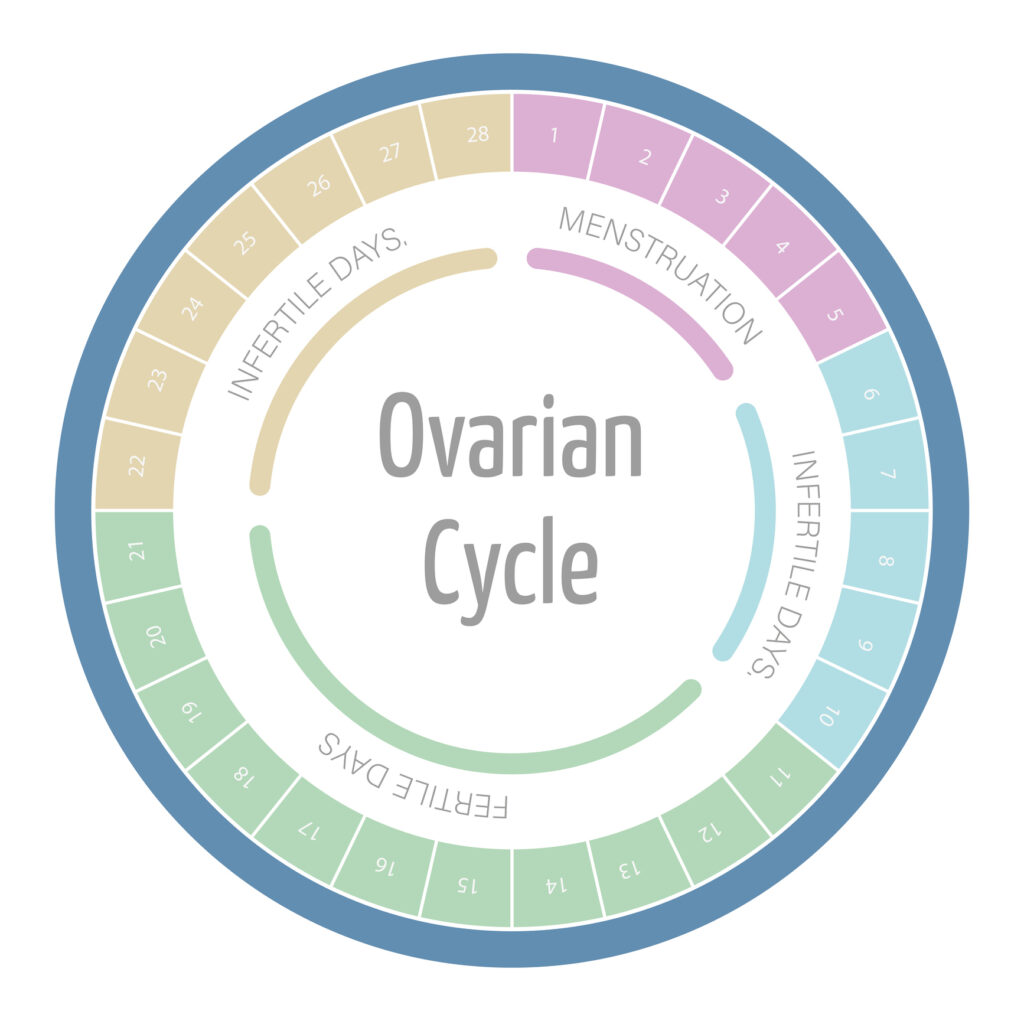
Research indicates that melatonin helps regulate the hypothalamic-pituitary-gonadal (HPG) axis, which controls reproductive hormone production. Disruption in melatonin levels can lead to imbalances in this axis, potentially affecting ovulation, sperm quality, and overall fertility. Melatonin has been shown to protect ovarian follicles from oxidative stress, a key factor in maintaining healthy egg quality. Studies suggest that melatonin may also play a role in the timing of puberty. Its levels fluctuate during different life stages. It indicates its importance in both the onset of reproductive capability and the maintenance of reproductive health throughout the lifespan.
Research findings on screen time and fertility outcomes
Emerging studies have begun to explore the link between excessive screen time at night, melatonin suppression, and reproductive health outcomes. A 2022 study published in the Journal of Endocrinology and Metabolism found that women with higher nighttime screen exposure exhibited altered menstrual cycles and reduced melatonin levels compared to those with limited screen use.
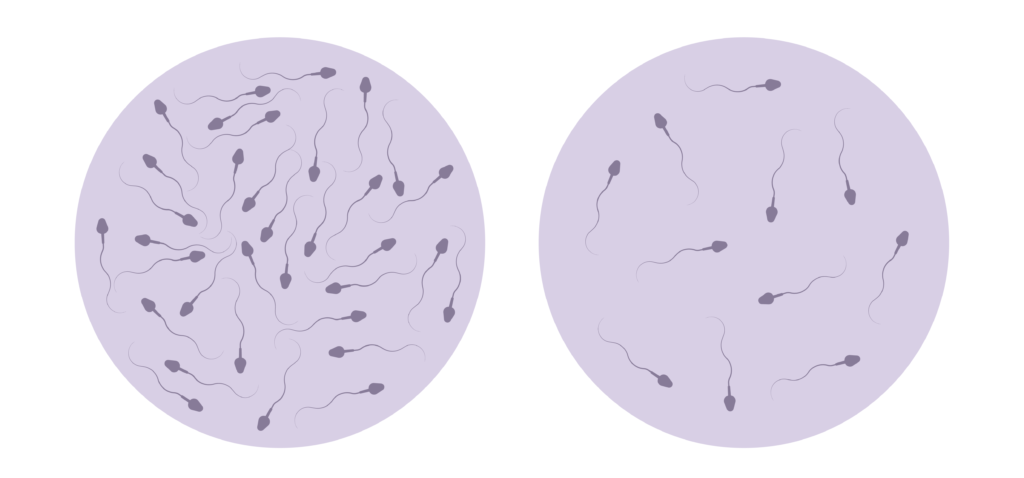
Research has demonstrated that disrupted sleep patterns and melatonin suppression correlate with lower testosterone levels and decreased sperm motility. The Centers for Disease Control and Prevention (CDC) reports that infertility affects approximately 12% of reproductive-aged couples in the United States, and lifestyle factors—including sleep hygiene and screen exposure—are increasingly recognized as contributing elements. Other lifestyle factors like diet, exercise, and stress management are also being investigated for their potential impact on melatonin production. For instance, a balanced diet rich in antioxidants and omega-3 fatty acids may support melatonin synthesis. While regular physical activity has been shown to enhance sleep quality, creating a more favorable environment for hormone regulation. These findings underscore the importance of a holistic approach to reproductive health, where lifestyle modifications can play a critical role in optimizing fertility outcomes.
Practical Solutions for Digital Wellness
Technology-based interventions (blue light filters, night mode apps)
Fortunately, technology itself offers tools to mitigate the negative effects of blue light exposure. Many devices now come equipped with built-in blue light filters or “night mode” settings that reduce the emission of blue wavelengths during evening hours. These modes typically shift screen colors toward warmer hues, which are less disruptive to melatonin production.
Additionally, specialized apps and software can adjust screen brightness and color temperature based on the time of day, automatically activating these protective settings at dusk. Blue light blocking glasses are another popular option, designed to filter out blue light wavelengths and protect the eyes during nighttime screen use. These glasses come in various styles and strengths, catering to different needs and preferences, making them a versatile choice for anyone looking to reduce eye strain. Some users report that wearing these glasses not only helps them sleep better but also reduces headaches associated with prolonged screen time, enhancing overall productivity during the day.
Behavioral changes to protect hormonal health at night
Beyond technological solutions, behavioral adjustments can significantly improve hormonal health and sleep quality. Experts recommend limiting screen time at least one to two hours before bedtime to allow melatonin levels to rise naturally. Establishing a relaxing pre-sleep routine—such as reading a physical book, practicing mindfulness, or engaging in gentle stretching—can help signal to the body that it is time to wind down.
Creating a sleep-friendly environment and maintaining a consistent sleep schedule also supports circadian rhythm stability. For individuals concerned about fertility or hormonal imbalances, consulting healthcare professionals about sleep hygiene and lifestyle habits is a prudent step toward holistic wellness. Furthermore, incorporating calming activities such as aromatherapy with essential oils like lavender or chamomile can enhance relaxation and create a soothing atmosphere conducive to sleep. Engaging in light yoga or meditation before bedtime can also help clear the mind, reducing anxiety and promoting a deeper, more restorative sleep cycle. By making these small yet impactful changes, individuals can foster a healthier relationship with technology while prioritizing their well-being.