Discover the overlooked sperm factors not shown in standard semen analysis. Learn key insights to improve fertility, with expert tips—boost your chances today!.
Beyond Basic Parameters: The Hidden Dimensions of Sperm Health
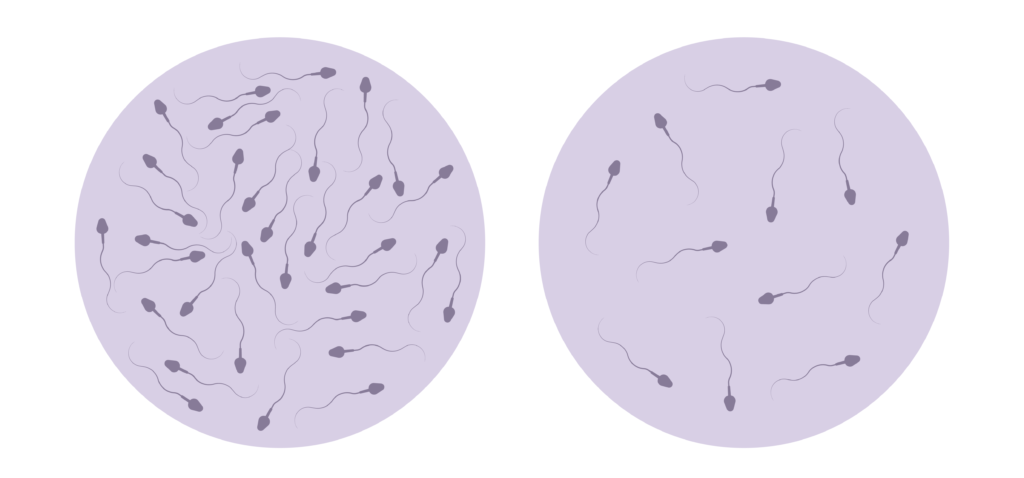
When evaluating male fertility, a standard semen analysis is often the first step. This test typically assesses sperm concentration, motility, morphology, and volume of the ejaculate. While these parameters provide valuable information, they only scratch the surface of sperm health. Many men with normal semen analysis results still face fertility challenges, indicating that critical factors remain unexamined in routine testing.
Understanding these hidden dimensions of sperm health is essential. Beyond the basic parameters, sperm quality encompasses molecular and functional aspects that influence fertilization success and embryo development. These ignored factors can provide deeper insights into male reproductive potential and guide more targeted interventions.
DNA Fragmentation and Chromatin Integrity
One of the most significant overlooked factors is sperm DNA fragmentation. Unlike the visible morphology or motility, DNA fragmentation refers to breaks or damage in the genetic material carried by sperm. High levels of DNA fragmentation have been linked to reduced fertilization rates, poor embryo quality, increased miscarriage risk, and lower pregnancy success even with assisted reproductive technologies (ART).
Chromatin integrity is closely related, showing how tightly the sperm DNA is packaged. Proper chromatin condensation protects the genetic material during transit and delivery to the egg. Abnormal chromatin packaging can compromise DNA stability, leading to fragmentation and impaired sperm function. Studies estimate that up to 30% of infertile men with normal semen analysis may have elevated DNA fragmentation. This highlights the importance of this parameter.
Testing for DNA fragmentation can be performed using assays. These include the TUNEL test, sperm chromatin structure assay (SCSA), or the comet assay. The Centers for Disease Control and Prevention (CDC) highlights the role of DNA integrity in reproductive health. This emphasizes that genetic quality is as crucial as sperm count and motility. Emerging research suggests that addressing DNA fragmentation through lifestyle modifications. Such as improved nutrition and stress management, could enhance sperm quality and overall reproductive outcomes.
Oxidative Stress and Free Radical Damage
Oxidative stress is another critical factor. It occurs when there is an imbalance between reactive oxygen species (ROS) and the body’s antioxidant defenses. While low levels of ROS are necessary for sperm capacitation and acrosome reaction, excessive ROS can damage sperm membranes, proteins, and DNA.
Free radical damage induced by oxidative stress can impair sperm motility, reduce viability, and increase DNA fragmentation. Lifestyle factors such as smoking, pollution exposure, poor diet, and infections can exacerbate oxidative stress. According to the National Institute of Child Health and Human Development (NICHD), oxidative stress is a leading cause of male infertility.
Measuring oxidative stress involves assays like chemiluminescence or flow cytometry to quantify ROS levels or assess antioxidant capacity. These tests can identify oxidative damage that might be mitigated through lifestyle changes, antioxidant therapy, or medical treatment. Certain dietary supplements, such as vitamins C and E, coenzyme Q10, and selenium, have shown promise in reducing oxidative stress. This growing body of evidence suggests that a proactive approach to managing oxidative stress could be a game-changer for men facing fertility issues.
Functional Capabilities Missing from Standard Analysis
Beyond molecular damage, sperm must perform specific functional tasks to achieve fertilization. Standard semen analysis does not evaluate these capabilities, which can be critical determinants of reproductive success. Functional assays assess the sperm’s ability to undergo physiological changes and interact with the egg. This provides a more complete picture of fertility potential. These assessments are essential not only for diagnosing male infertility but also for optimizing treatment strategies.

Capacitation and Acrosome Reaction Potential
Capacitation is a biochemical process sperm undergo after ejaculation, allowing them to fertilize the egg. This involves changes in membrane fluidity, ion channel activity, and protein phosphorylation. The acrosome reaction, which follows capacitation, is the release of enzymes from the sperm’s acrosome that allows penetration of the egg’s protective layers. Understanding these processes is crucial, as they are not merely biological events but rather finely tuned mechanisms that ensure successful fertilization.
Standard semen analysis does not measure a sperm’s ability to undergo the acrosome reaction. Deficiencies in these processes can result in fertilization failure despite normal sperm count and motility. Specialized tests, such as the chlortetracycline (CTC) fluorescence assay or acrosome reaction assays, evaluate these functional capacities. By identifying specific deficiencies, clinicians can provide targeted interventions, potentially improving the chances of conception through assisted reproductive technologies.
Identifying defects in capacitation or acrosome reaction can guide treatment decisions, including the use of intracytoplasmic sperm injection (ICSI) in assisted reproduction, where a single sperm is injected directly into the egg, bypassing these functional requirements. This approach not only addresses the immediate issue of fertilization but also opens up discussions about the underlying causes of sperm dysfunction, which may include genetic factors, environmental influences, or lifestyle choices.
Zona Pellucida Binding Efficiency
Another overlooked functional parameter is the sperm’s ability to bind to the zona pellucida, the glycoprotein layer surrounding the egg. This binding is a critical step for sperm recognition and penetration, initiating fertilization. Standard semen analysis does not assess this interaction, which depends on specific receptors and membrane proteins on the sperm surface. The complexity of this interaction highlights the importance of understanding sperm-egg communication, which is essential for successful fertilization and subsequent embryo development.
Zona pellucida binding assays (ZBA) measure the number of sperm that can attach to isolated zona pellucida or artificial substrates mimicking it. Poor binding efficiency has been associated with infertility and may not correlate with traditional semen parameters. This test can help differentiate between idiopathic infertility cases and guide appropriate ART techniques. Moreover, the implications of binding efficiency extend beyond the initial fertilization event; they may also influence the quality of the embryo and its ability to implant successfully in the uterine lining.
Advanced Diagnostic Approaches for Comprehensive Sperm Assessment
As the limitations of standard semen analysis become increasingly apparent, advanced techniques are emerging to provide a more holistic evaluation of sperm health. These approaches integrate molecular, functional, genetic, and epigenetic assessments to uncover hidden causes of male infertility. The need for such comprehensive assessments is highlighted by the rising frequency of male infertility, which affects approximately 15% of couples trying to conceive. Understanding the multifaceted nature of sperm health is crucial for developing targeted interventions and improving reproductive outcomes.
Emerging Technologies in Sperm Function Testing
Recent advances in technology have allowed the development of sophisticated sperm function tests. Microfluidic devices, for example, can isolate highly motile and morphologically normal sperm, mimicking natural selection processes within the female reproductive tract. This technology improves the selection of sperm for use in ART, potentially enhancing success rates. By creating an environment that simulates the conditions of the female reproductive system, these devices not only enhance sperm selection but also provide insights into the dynamic interactions between sperm and oocyte, paving the way for more effective fertilization techniques.
High-resolution imaging techniques, such as electron microscopy and advanced fluorescence microscopy, allow detailed visualization of sperm ultrastructure and functional markers. These tools can detect subtle abnormalities in the sperm membrane, mitochondria, or acrosome that standard microscopy might miss. Furthermore, the integration of artificial intelligence with imaging technologies is revolutionizing sperm analysis by allowing automated assessments that enhance accuracy and reduce human error. This synergy between technology and biology holds promise for refining diagnostic criteria and improving the understanding of sperm functionality in various contexts.
Additionally, proteomic and metabolomic analyses are being explored to identify biomarkers of sperm function and fertility potential. These approaches analyze the protein and metabolic profiles of sperm cells, offering insights into their physiological status and capacity to support fertilization and embryo development. By identifying specific protein expressions and metabolic pathways that correlate with successful fertilization, researchers aim to develop novel diagnostic tools and therapeutic strategies that could significantly improve the management of male infertility.
Integrating Genetic and Epigenetic Sperm Evaluation
Beyond DNA fragmentation, comprehensive genetic and epigenetic evaluation of sperm is gaining attention. Genetic testing can identify chromosomal abnormalities, microdeletions, or mutations that may impact fertility or lead to inherited conditions. These tests are particularly relevant for men with severe oligospermia or azoospermia. The implications of such genetic insights extend beyond immediate fertility concerns, as they can inform couples about potential genetic risks for their offspring, allowing for more informed reproductive choices.
Epigenetic modifications, such as DNA methylation and histone modifications, regulate gene expression without altering the DNA sequence. Aberrant epigenetic patterns in sperm have been linked to infertility, poor embryo development, and even long-term health effects in offspring. Research is ongoing to develop reliable epigenetic assays for clinical use. The exploration of how environmental factors, lifestyle choices, and even paternal age can influence epigenetic markers in sperm adds another layer of complexity to fertility assessments. Understanding these influences may lead to preventive strategies that enhance sperm quality and overall reproductive health.
Integrating genetic and epigenetic data with traditional semen analysis and functional testing offers a comprehensive approach to male fertility assessment. This holistic view can improve diagnosis, treatment, and ultimately enhance reproductive outcomes for couples facing infertility. As the field continues to evolve, the collaboration between reproductive endocrinologists, geneticists, and molecular biologists will be essential in translating these advanced diagnostic techniques into clinical practice, ensuring that couples receive the most effective care possible.