Discover how someone can have endometriosis without obvious symptoms and learn the key clues to identify it.
Understanding Silent Endometriosis
Endometriosis is a chronic condition where endometrium, grows outside the uterus. It affects an estimated 1 in 10 women of reproductive age worldwide. This is according to the Centers for Disease Control and Prevention (CDC). While many associate endometriosis with severe pelvic pain and heavy menstrual bleeding, a significant number of individuals experience little to no obvious symptoms. This phenomenon is often referred to as “silent” or asymptomatic endometriosis.

Silent endometriosis challenges traditional perceptions of the disease. The absence of classic symptoms can delay diagnosis and treatment, sometimes for years. Understanding how endometriosis can exist without the hallmark signs is crucial for both patients and healthcare providers. It also highlights the importance of recognizing subtle clues and patterns that might otherwise be overlooked. In fact, some women report vague symptoms like fatigue, gastrointestinal issues, or even unexplained infertility. These can easily be dismissed or attributed to other health concerns. This complexity adds to the challenge of obtaining timely and accurate diagnoses.
The Spectrum of Endometriosis Symptoms
Endometriosis symptoms vary widely, ranging from debilitating pain to no symptoms at all. Commonly reported symptoms include dysmenorrhea (painful periods), chronic pelvic pain, painful intercourse, and infertility. However, the intensity and presence of symptoms do not always correlate with the extent of the disease. Some individuals with extensive endometrial lesions may report minimal discomfort, while others with milder forms suffer severe pain.
This variability is partly due to the location and depth of endometrial implants, individual pain thresholds, and the body’s inflammatory response. For example, superficial lesions on the peritoneum might cause less pain than deeply infiltrating endometriosis affecting nerves or organs. Additionally, some lesions might not provoke significant inflammation, resulting in fewer symptoms. This discrepancy can lead to a false sense of security for those with silent endometriosis, as they may not realize the potential long-term implications of the condition, including the risk of developing adhesions or other complications that could affect reproductive health.
Why Some Cases Go Undetected for Years
Endometriosis without obvious symptoms often remains undiagnosed because the condition is typically suspected based on clinical symptoms. Without pain or menstrual irregularities, individuals may not seek medical advice, and routine gynecological exams might not reveal the disease. Furthermore, endometriosis can only be definitively diagnosed through laparoscopy, a surgical procedure, which is usually reserved for symptomatic cases.
Another factor contributing to delayed detection is the overlap of endometriosis symptoms with other conditions such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID). When symptoms are mild or nonspecific, they may be attributed to these more common disorders, leading to misdiagnosis or underdiagnosis. This underscores the need for heightened awareness and vigilance even when classic symptoms are absent. Moreover, the stigma surrounding menstrual health and reproductive issues can prevent individuals from discussing their experiences openly. This further complicates the path to diagnosis. Education and advocacy are essential to empower those affected to seek help and to foster a more informed dialogue between patients and healthcare providers.
Subtle Signs You Should not Ignore
Recognizing silent endometriosis requires attention to subtle signs that might otherwise be dismissed. These signs often do not fit the typical profile of the disease but can provide important clues to its presence. Awareness of these subtle indicators is essential for early intervention and improved outcomes.
Non-Specific Symptoms Often Attributed to Other Conditions
Many individuals with silent endometriosis report symptoms that are vague or non-specific, such as fatigue, mild digestive issues, or intermittent pelvic discomfort. These symptoms can easily be mistaken for stress, dietary problems, or hormonal fluctuations. For instance, bloating and constipation are common complaints that overlap with gastrointestinal disorders. This can make it difficult to pinpoint endometriosis without further investigation.
Additionally, some may experience subtle changes in menstrual patterns, like slightly heavier or irregular periods, without pain. These changes can be overlooked or attributed to normal hormonal variations. Recognizing that these non-specific symptoms might be related to endometriosis requires a comprehensive approach to patient history and symptom evaluation. Moreover, the emotional toll of these symptoms can be significant. This leads to feelings of frustration or anxiety as individuals struggle to understand their bodies. This emotional aspect can further complicate the recognition of endometriosis, as individuals may dismiss their symptoms as mere stress or anxiety rather than seeking medical advice.
Cyclical Patterns and Timing Clues
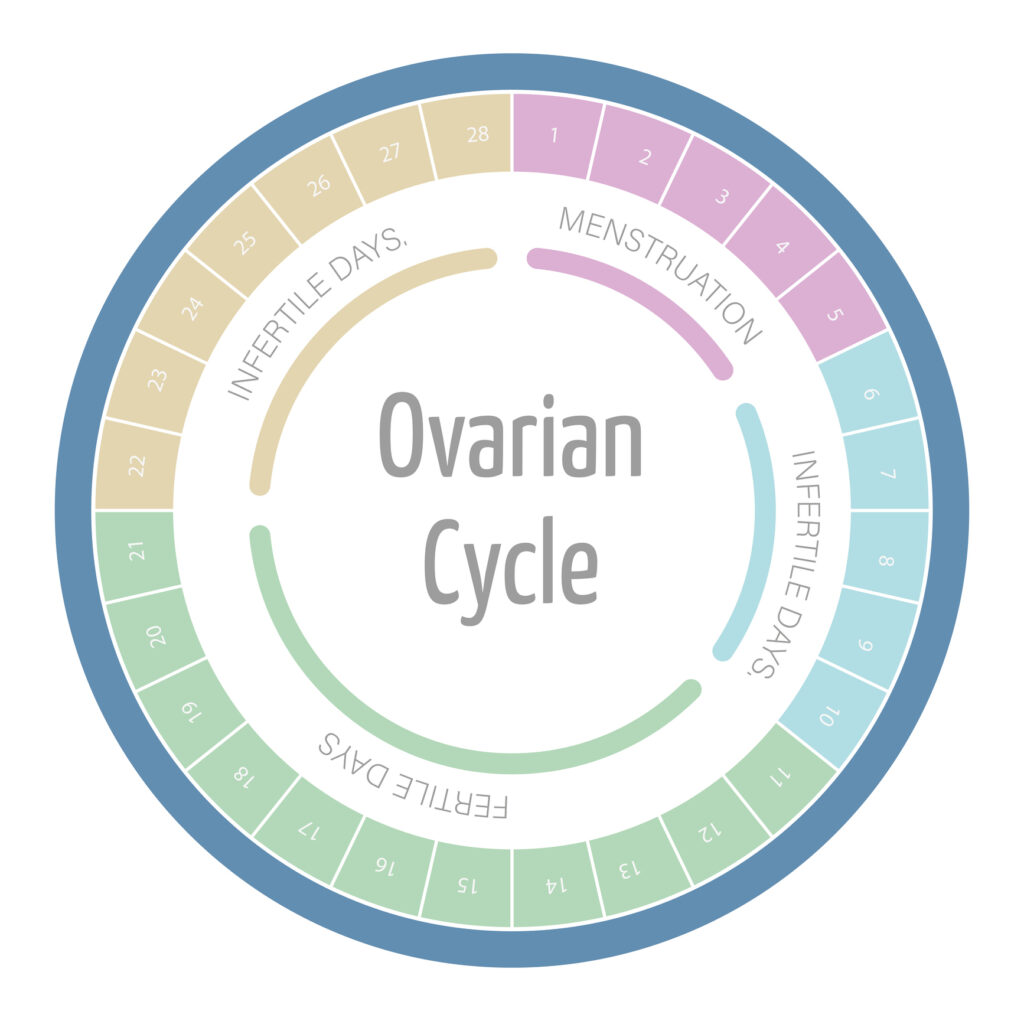
One important clue to silent endometriosis lies in the cyclical nature of symptoms. Some individuals notice that certain symptoms worsen or appear in relation to their menstrual cycle. For example, mild digestive discomfort or fatigue might intensify during menstruation or ovulation.
These cyclical patterns suggest hormonal influences on endometrial lesions outside the uterus. These respond to the menstrual cycle similarly to uterine lining. Tracking symptoms over several months can reveal these patterns, prompting further evaluation. This approach is especially valuable when symptoms are subtle and inconsistent. Additionally, keeping a detailed symptom diary can empower individuals to articulate their experiences more clearly during medical consultations. This can potentially leading to more accurate diagnoses. Engaging in this proactive measure not only enhances self-awareness but also fosters a collaborative relationship with healthcare providers, paving the way for tailored treatment options that address the unique manifestations of silent endometriosis.
Detection and Diagnosis of Asymptomatic Endometriosis
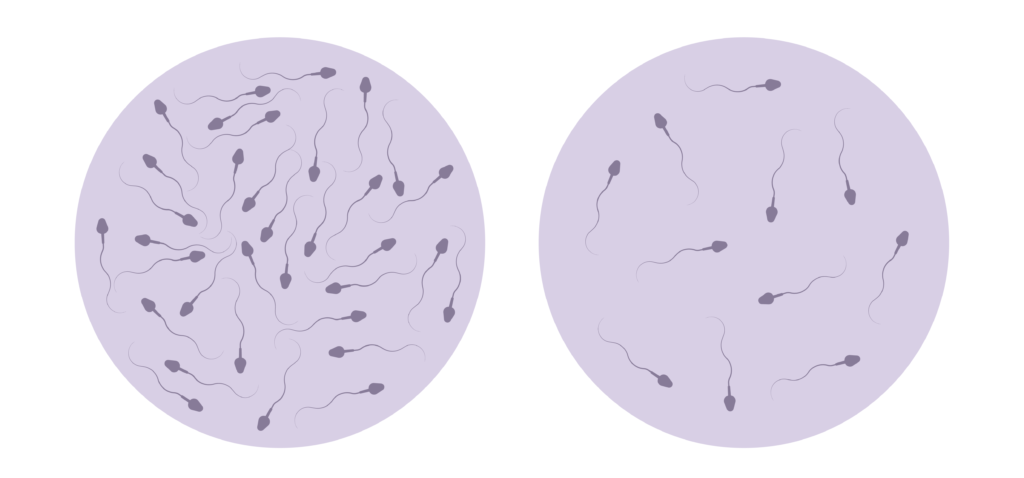
Diagnosing endometriosis in the absence of obvious symptoms is challenging but increasingly feasible with advances in medical technology and clinical awareness. Early detection is important to prevent disease progression and associated complications such as infertility.
Modern Diagnostic Approaches Beyond Symptom Assessment
Traditionally, laparoscopy has been the gold standard for diagnosing endometriosis, allowing direct visualization and biopsy of lesions. However, this invasive procedure is not practical for screening asymptomatic individuals. Instead, non-invasive imaging techniques such as transvaginal ultrasound and magnetic resonance imaging (MRI) are gaining prominence in detecting endometriotic cysts and deep infiltrating lesions.
Emerging research is also exploring biomarkers in blood, urine, and menstrual fluid that could signal the presence of endometriosis. While no definitive biomarker has yet been established for routine clinical use, these developments hold promise for earlier and less invasive diagnosis in the future. The identification of specific proteins or genetic markers associated with endometriosis could revolutionize how the condition is diagnosed, potentially allowing for a simple blood test that could be administered during routine check-ups.
When to Seek Medical Evaluation Even Without Pain
It is important to consider medical evaluation for endometriosis even in the absence of classic symptoms, particularly if there are risk factors or subtle signs present. Individuals experiencing unexplained infertility, cyclical digestive issues, or persistent fatigue should discuss these concerns with their healthcare provider.
Additionally, those with a family history of endometriosis or other gynecological conditions may benefit from proactive screening. Early consultation can facilitate timely diagnosis and management, improving quality of life and reproductive outcomes. Furthermore, awareness campaigns aimed at educating the public about the potential for asymptomatic endometriosis are crucial. These initiatives can empower individuals to advocate for their health and seek evaluations, even when they do not experience the hallmark symptoms typically associated with the disease. By fostering an environment where patients feel comfortable discussing their concerns, healthcare providers can better identify and address endometriosis in its silent forms.
In conclusion, endometriosis can exist without obvious symptoms, making awareness of subtle clues essential. Understanding the spectrum of symptoms, recognizing non-specific signs, and utilizing modern diagnostic tools can help identify silent endometriosis. If there are any concerns or unusual patterns, seeking medical advice is a critical step toward effective care.