Discover the surprising advantages of using Clomiphene Citrate 50 mg for men, from enhanced fertility to increased testosterone levels.
The Benefits of Clomiphene Citrate 50 mg for Men
Clomiphene citrate is a medication commonly used in women to treat infertility. However, recent research has revealed its potential benefits for men as well. In this article, we will explore the various advantages of Clomiphene Citrate 50 mg for men and delve into its role in men’s health.
Understanding Clomiphene Citrate
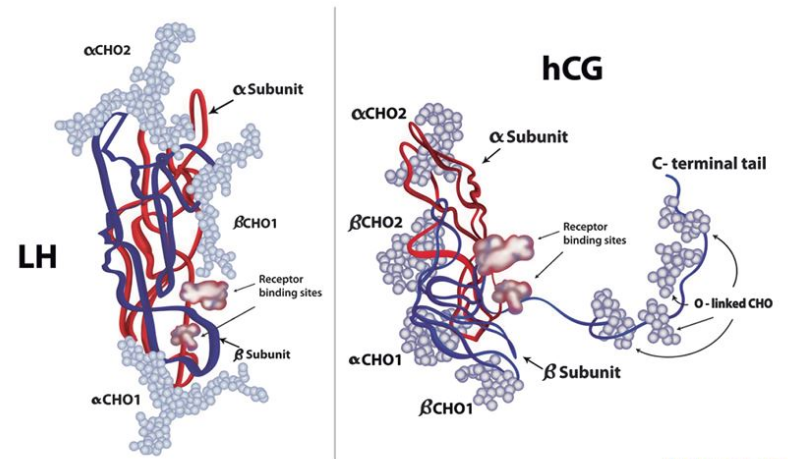
Clomiphene Citrate, also known as Clomid, is a selective estrogen receptor modulator (SERM) that acts as a potent anti-estrogen. It blocks the effects of estrogen in the body, which can lead to increased production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones are crucial for stimulating the testes to produce testosterone and promote sperm production.
Clomid is commonly prescribed to both men and women for different reasons. In women, it is often used to induce ovulation in cases of infertility, while in men, it is utilized to boost testosterone levels and enhance fertility. This versatility in treating hormonal imbalances has made Clomiphene Citrate a popular choice among healthcare providers.
What is Clomiphene Citrate?
Clomiphene citrate is a synthetic drug that was initially developed to stimulate ovulation in women struggling with fertility issues. However, it has also been found to have beneficial effects in men by boosting testosterone levels and improving fertility.

When it comes to male fertility, Clomid can be a game-changer for individuals experiencing low testosterone levels or issues with sperm production. By targeting the hormonal pathways that influence testosterone synthesis, Clomiphene Citrate can help restore hormonal balance and improve overall reproductive health.
How Does Clomiphene Citrate Work?
Clomiphene Citrate works by interacting with the hypothalamus in the brain, which plays a crucial role in regulating hormone production. By blocking estrogen receptors in the hypothalamus, it increases the release of GnRH (gonadotropin-releasing hormone). This, in turn, stimulates the pituitary gland to secrete more FSH and LH, leading to an increase in testosterone production.
By understanding the intricate mechanisms of action of Clomiphene Citrate, healthcare providers can tailor treatment plans to address specific hormonal imbalances effectively. This personalized approach ensures that individuals receive the most appropriate care to optimize their reproductive health and overall well-being.
The Role of Clomiphene Citrate in Men’s Health
Clomiphene Citrate, a medication commonly used in the treatment of female infertility, has also shown promising results in improving men’s health. While its mechanism of action was initially developed to aid women in ovulation, its impact on men’s health has gained recognition in recent years.
Now that we understand how Clomiphene Citrate works, let’s delve deeper into its specific benefits for men’s health, beyond just its traditional use.
Clomiphene Citrate and Testosterone Levels
Testosterone, often referred to as the “male hormone,” plays a crucial role in various aspects of men’s health, including the maintenance of muscle mass, bone density, and libido. Low testosterone levels can result in a myriad of health issues such as fatigue, decreased libido, and reduced muscle strength. Clomiphene Citrate acts as a selective estrogen receptor modulator in men, stimulating the testes to produce more testosterone. By restoring testosterone levels, this medication effectively alleviates the symptoms associated with low testosterone, leading to an improvement in overall well-being.
Impact on Male Fertility
Male fertility is another area where Clomiphene Citrate has demonstrated significant benefits. For men facing fertility challenges due to factors such as low sperm count or poor sperm motility, this medication offers a potential solution. By increasing the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), Clomiphene Citrate promotes spermatogenesis and enhances sperm quality. These improvements not only boost male fertility but also increase the chances of achieving a successful pregnancy, providing hope to couples struggling with infertility.
Dosage and Administration of Clomiphene Citrate
As with any medication, it is essential to follow the recommended dosage and administration guidelines for Clomiphene Citrate to ensure optimal results.
Clomiphene Citrate, commonly known by its brand name Clomid, is a medication often prescribed to treat infertility in women. However, it is also used off-label in men to help increase testosterone levels. Understanding the proper dosage and administration of Clomiphene Citrate is crucial for its effectiveness in addressing hormonal imbalances and fertility issues.
Recommended Dosage for Men
The typical starting dose of Clomiphene Citrate for men is 25 mg per day. However, depending on individual response and testosterone levels, the dosage can be adjusted up to 50 mg per day. It is crucial to work closely with a healthcare professional, such as an endocrinologist or urologist, to determine the most appropriate dosage for your specific needs. Factors such as age, weight, underlying health conditions, and treatment goals will all play a role in determining the optimal dosage of Clomiphene Citrate.
Proper Administration and Timing
Clomiphene Citrate is typically taken orally for a specific duration, usually ranging from 4 to 6 months. It is advisable to take the medication at the same time each day to ensure consistency and maximize its effectiveness. While some individuals may experience improvements in testosterone levels and fertility within a few weeks of starting treatment, it is essential to continue taking Clomiphene Citrate for the prescribed duration to achieve long-lasting results. Regular monitoring of testosterone levels through blood tests is also recommended to assess the effectiveness of the treatment and make any necessary dosage adjustments.
Potential Side Effects and Risks
While Clomiphene Citrate is generally well-tolerated, it is essential to be aware of potential side effects and address any concerns with your healthcare provider.
Clomiphene Citrate, commonly prescribed for its ovulation-inducing properties in women, is also used off-label in men to treat infertility. The medication works by stimulating the release of hormones necessary for sperm production. Despite its effectiveness, some users may experience side effects that warrant attention.
Common Side Effects in Men
Some men may experience side effects such as hot flashes, mood swings, and headaches. These side effects are typically mild and subside over time. However, it is essential to communicate any persistent or severe side effects to your healthcare provider.
In addition to the common side effects mentioned, some men may also report visual disturbances or changes in libido while taking Clomiphene Citrate. These symptoms are usually temporary and reversible upon discontinuation of the medication. It is crucial to monitor and report any unusual changes in your health while undergoing treatment.
Addressing Potential Risks and Concerns
Clomiphene Citrate is generally safe when used under medical supervision. However, individuals with certain medical conditions, such as liver disease or a history of blood clots, may require special monitoring. It is crucial to disclose your medical history and any ongoing medications to your healthcare provider before starting Clomiphene Citrate.
Your healthcare provider will evaluate your individual risk factors and tailor a treatment plan that maximizes benefits while minimizing potential risks. Regular monitoring and open communication with your healthcare team are essential to ensure the safe and effective use of Clomiphene Citrate for your specific needs.
The Effectiveness of Clomiphene Citrate 50 mg
Now that we have explored the benefits and potential risks of Clomiphene Citrate, let’s delve into its effectiveness and long-term outcomes.
Evaluating the Success Rate
Studies have shown varying success rates for Clomiphene Citrate in improving testosterone levels and fertility in men. While some individuals may experience significant improvements, others may have a more modest response. Factors such as individual physiology, underlying health conditions, and adherence to dosage and administration guidelines can influence the overall effectiveness.
Long-Term Benefits and Outcomes
When used as prescribed and under medical supervision, Clomiphene Citrate can provide long-term benefits for men struggling with low testosterone levels or fertility issues. Improved testosterone levels can positively impact overall well-being, including increased energy levels, improved mood, and enhanced sexual function.
Furthermore, research has suggested that Clomiphene Citrate may also have potential benefits beyond its primary indications. Some studies have explored its use in enhancing athletic performance, particularly in male athletes looking to boost their testosterone levels within permissible limits. While more research is needed in this area, the preliminary findings hint at the diverse applications of this medication.
It’s essential to note that like any medication, Clomiphene Citrate may not be suitable for everyone. Individuals with certain medical conditions or those taking specific medications may not be ideal candidates for this treatment. Consulting with a healthcare provider to assess individual suitability and closely monitoring any side effects or changes during treatment is crucial for maximizing the benefits of Clomiphene Citrate.
Conclusion
In conclusion, Clomiphene Citrate 50 mg offers several benefits for men’s health, including increased testosterone levels and improved fertility. However, it is crucial to consult with a healthcare professional to determine the appropriate dosage, monitor potential side effects, and evaluate the overall effectiveness of the treatment. With proper medical guidance, Clomiphene Citrate can be a valuable tool in addressing hormonal imbalances and enhancing men’s overall health and well-being.