Explore the potential side effects of HCG in males and gain valuable insights into its impact on men’s health.
The Side Effects of HCG for Men
In recent years, the use of HCG (Human Chorionic Gonadotropin) has gained popularity among males for various purposes, including weight loss, muscle building, and boosting testosterone levels. However, it is important to understand that HCG, like any medication, can have side effects. In this article, we will delve into the potential side effects of HCG for men and discuss their implications on health and well-being.
Understanding HCG: An Overview
Before exploring its side effects, let’s first understand how HCG works and its role in the male body. HCG is a hormone produced during pregnancy by the placenta. In males, it is naturally produced in small amounts by the testes. It plays a crucial role in stimulating testosterone production and supporting fertility.
What is HCG?
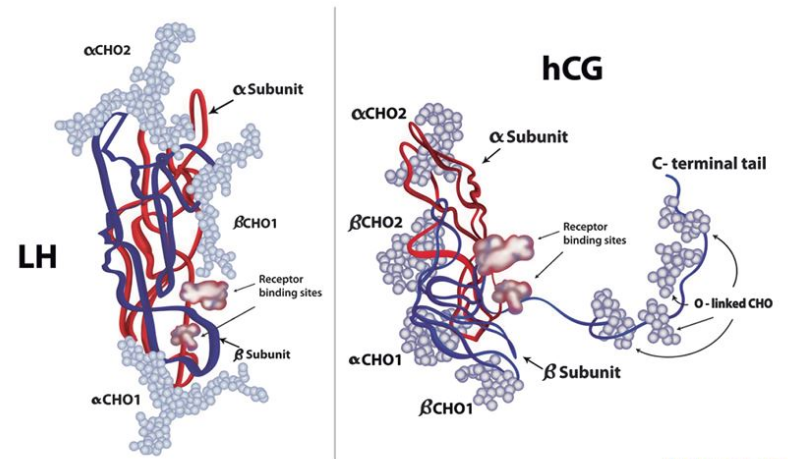
HCG, short for Human Chorionic Gonadotropin, is a hormone that is typically associated with pregnancy. It is produced by the placenta and helps regulate hormone levels during pregnancy. In males, HCG is also present, albeit in smaller amounts, and serves important functions related to fertility and testosterone production.
The Role of HCG in the Male Body
Within the male body, HCG plays a crucial role in stimulating the production of testosterone, the primary male sex hormone. It acts as a luteinizing hormone that signals the testes to produce more testosterone. Additionally, HCG also supports the health and functioning of the testes, helping to maintain fertility and sperm production.
Furthermore, HCG has been utilized in various medical treatments beyond its natural functions. One common use of HCG is in the treatment of infertility issues in men. By boosting testosterone levels and supporting sperm production, HCG injections can help improve fertility outcomes for men struggling with low sperm counts or other reproductive challenges.
It is important to note that while HCG is beneficial in certain medical contexts, its misuse can lead to adverse effects. Athletes and bodybuilders have been known to abuse HCG for its purported ability to enhance performance and aid in weight loss. However, such off-label use of HCG can disrupt hormonal balance and have detrimental effects on overall health.
The Medical Use of HCG in Males
While HCG is primarily associated with its role in pregnancy, it also has medical applications for males. One such use is in treating infertility.
Aside from its well-known role in pregnancy, human chorionic gonadotropin (HCG) has garnered attention for its therapeutic benefits in males. Beyond its traditional use in fertility treatments for women, HCG has shown promise in addressing various health concerns in men, particularly in the realm of reproductive health.
Treating Infertility with HCG
In cases of male infertility, where testosterone levels are low, HCG can be prescribed as part of a treatment regimen to stimulate testosterone production. This can improve the chances of achieving pregnancy and assist in overcoming certain hormonal imbalances that contribute to infertility.
Male infertility is a complex issue that can stem from various factors, including hormonal imbalances and physiological abnormalities. HCG therapy offers a targeted approach to addressing these underlying issues, providing a potential solution for couples struggling with conception.
HCG and Testosterone Production
HCG has also been used off-label to increase testosterone levels in males with conditions such as hypogonadism. By stimulating the testes, HCG can enhance testosterone production, leading to improved libido, energy levels, and muscle mass. However, it is crucial to highlight that the efficacy of HCG for testosterone enhancement is still a topic of debate among medical professionals.
While HCG’s role in boosting testosterone levels has shown promising results in some studies, the long-term effects and optimal dosages remain areas of ongoing research. As the medical community continues to explore the potential benefits and risks of HCG therapy for testosterone enhancement, it underscores the importance of individualized treatment plans tailored to each patient’s unique needs and health profile.
Potential Side Effects of HCG in Males
While HCG may provide some potential benefits, it is essential to be aware of the potential side effects that can occur with its use. These side effects can be both physical and psychological in nature.
Human Chorionic Gonadotropin (HCG) is a hormone that is naturally produced in the placenta during pregnancy. In males, HCG is sometimes used to treat testosterone deficiency or to aid in weight loss. However, like any medication or hormone therapy, there are potential risks and side effects associated with its use.
Physical Side Effects
Some individuals may experience physical side effects when using HCG. These can include headaches, fatigue, swelling or pain at the injection site (if HCG is administered via injection), and water retention. Additionally, there have been reports of gynecomastia, also known as “man boobs,” as a potential side effect. It is important to note that the incidence and severity of these physical side effects may vary from person to person.
Furthermore, HCG can also lead to other physical side effects such as acne, edema (swelling caused by excess fluid trapped in your body’s tissues), and an increased risk of blood clots. It is crucial for individuals considering HCG therapy to consult with a healthcare provider to discuss these potential physical side effects and weigh them against the benefits of treatment.
Psychological Side Effects
In addition to physical side effects, some individuals may experience psychological side effects when using HCG. These can include mood swings, irritability, and changes in libido. It is worth noting that these psychological side effects can be impacted by individual factors such as pre-existing mental health conditions or the misuse of HCG in unregulated doses.
Moreover, some individuals may also experience anxiety, depression, or insomnia as psychological side effects of HCG therapy. These effects can be particularly challenging for individuals already struggling with mental health issues. It is crucial for healthcare providers to monitor patients closely for any signs of psychological distress while undergoing HCG treatment.
The Long-Term Impact of HCG Use
While the short-term side effects of HCG are important to consider, it is equally important to understand the potential long-term impact of its use. The use of HCG may affect hormonal balance and overall health in several ways.
Delving deeper into the long-term implications of HCG use reveals a complex interplay between synthetic hormones and the body’s natural regulatory systems. Exogenous HCG supplementation can disrupt the delicate balance of hormones within the body, leading to potential repercussions that extend far beyond the initial use period. It is crucial to recognize that the effects of HCG on hormonal balance may not be immediately apparent and could manifest gradually over time.
Effects on Hormonal Balance
Exogenous HCG supplementation can disrupt the body’s natural hormonal balance. By introducing synthetic HCG into the system, the body’s feedback mechanisms for hormone production may be altered. Prolonged use or abuse of HCG may result in the suppression of natural testosterone production and potential complications with the hypothalamic-pituitary-gonadal (HPG) axis, which regulates hormone levels.
Furthermore, the intricate web of interactions between hormones can be further complicated by the introduction of exogenous HCG. The potential long-term consequences of disrupting hormonal balance extend beyond just testosterone levels, impacting various physiological processes that rely on a harmonious interplay of hormones.
Impact on Overall Health
While the impact of HCG on overall health is still being studied, there is concern that prolonged HCG use may have adverse effects on cardiovascular health, cholesterol levels, and liver function. Additionally, the use of HCG without proper medical supervision may increase the risk of developing complications or interactions with other medications.
Understanding the broader implications of HCG use on overall health necessitates a comprehensive evaluation of its potential systemic effects. From cardiovascular implications stemming from altered lipid profiles to the intricate relationship between hormonal disruptions and liver function, the long-term impact of HCG extends beyond isolated physiological systems, highlighting the need for thorough monitoring and research in this area.
Mitigating the Side Effects of HCG
If you are considering using HCG for its potential benefits, it is crucial to approach its use responsibly and with proper medical guidance. Here are some strategies to help mitigate the potential side effects:
Human Chorionic Gonadotropin (HCG) is a hormone that is often used in conjunction with a low-calorie diet to promote weight loss. While it can be effective for some individuals, it is essential to be aware of the potential side effects that may arise from its use. These side effects can range from mild to severe and may include headaches, fatigue, irritability, and swelling at the injection site.
Dosage and Side Effects
Ensure that you are using the correct dosage of HCG as prescribed by a qualified healthcare professional. Strictly following the recommended dosage can minimize the risk of experiencing severe side effects. It is important not to exceed the prescribed dose or use HCG without proper medical supervision.
Monitoring your body’s response to the hormone is crucial in identifying any adverse reactions early on. Keeping a journal of your symptoms and discussing them with your healthcare provider can help tailor your treatment plan for optimal results while minimizing potential risks.
Lifestyle Changes to Minimize Side Effects

Adopting a healthy lifestyle can go a long way in minimizing the potential side effects of HCG. Regular exercise, a balanced diet, adequate hydration, and stress management can support overall well-being. Additionally, open communication with medical professionals can help address any concerns or possible adjustments needed in the treatment plan.
It is important to recognize that while HCG may aid in weight loss, it is not a magic solution. Combining its use with sustainable lifestyle changes can lead to better long-term outcomes and reduce the likelihood of experiencing adverse effects. Prioritizing your health and well-being throughout the HCG treatment process is key to achieving your desired goals safely and effectively.
Conclusion
When considering the use of HCG in males, it is essential to weigh the potential benefits against the possible side effects. While HCG may offer some advantages, particularly when used under medical supervision for specific conditions, it is crucial to approach its use responsibly and with thorough understanding. Always consult with a qualified healthcare professional before beginning any HCG regimen to ensure it is appropriate for your individual needs and to minimize any potential risks or side effects.