Discover everything you need to know about the expenses associated with infertility treatment in this comprehensive guide.
Infertility is a challenging and emotional journey that affects millions of couples worldwide. For those who seek medical assistance to conceive, understanding the cost of infertility treatment is a crucial aspect of their decision-making process. In this comprehensive guide, we will delve into the various factors that contribute to the overall cost of infertility treatment, as well as available financial assistance and support options.
Understanding Infertility
Before delving into the cost aspect, it is essential to comprehend what infertility entails. Infertility is defined as the inability to conceive after a year of regular, unprotected intercourse for women under the age of 35, or after six months for women over 35. It affects both men and women, and various factors can contribute to its occurrence.
Infertility can be a complex and emotionally challenging journey for couples who are trying to conceive. It is important to understand the medical perspective of infertility to navigate through this difficult process.
Defining Infertility: A Medical Perspective
From a medical perspective, infertility is often classified as primary or secondary. Primary infertility refers to couples who have never been able to achieve a pregnancy, while secondary infertility affects couples who have successfully conceived in the past but struggle to conceive subsequently.
Primary infertility can be caused by a variety of factors, including issues with ovulation, sperm production, or the fallopian tubes. Secondary infertility, on the other hand, can be caused by changes in reproductive health over time, such as age-related decline in fertility or the development of health conditions that affect fertility.
It is important to note that infertility is not solely a female issue. Men can also contribute to infertility through factors such as low sperm count, poor sperm motility, or structural abnormalities in the reproductive system.
Common Causes of Infertility in Men and Women
Infertility can result from numerous factors, including hormonal imbalances, anatomical abnormalities, genetic disorders, age-related decline in fertility, or lifestyle choices such as smoking or excessive alcohol consumption. Both men and women can contribute to infertility, and a thorough diagnostic evaluation is essential to determine the underlying cause.
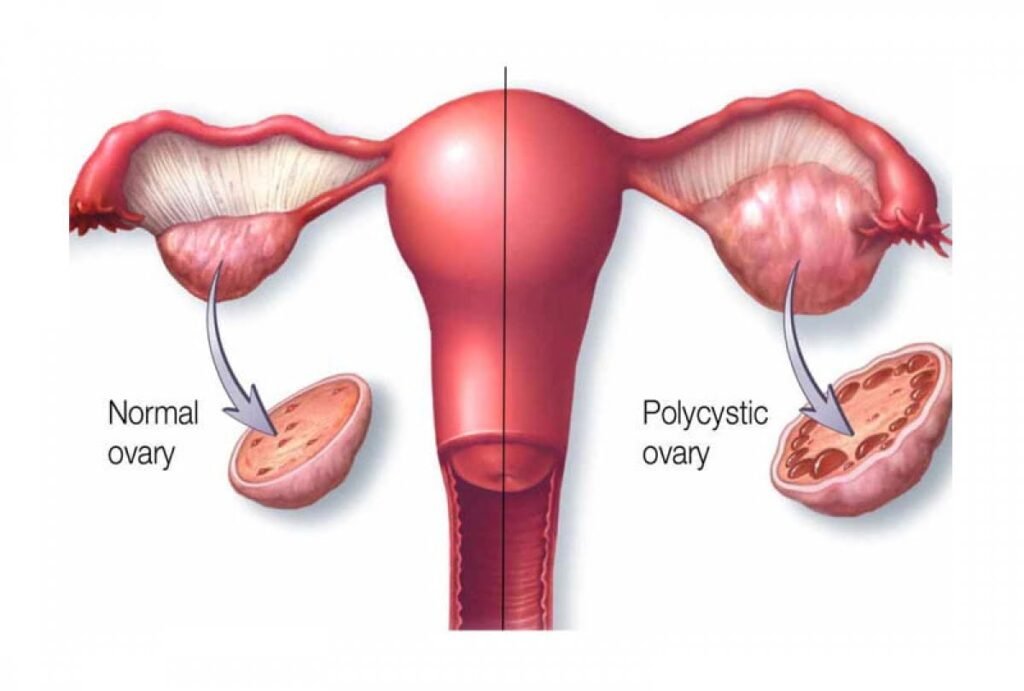
Hormonal imbalances can disrupt the delicate balance necessary for successful conception. In women, conditions such as polycystic ovary syndrome (PCOS) or thyroid disorders can affect ovulation and hormone production. In men, hormonal imbalances can affect sperm production and quality.
Anatomical abnormalities, such as blocked fallopian tubes in women or structural issues in the male reproductive system, can also contribute to infertility. These issues can prevent the sperm from reaching the egg or the fertilized egg from implanting in the uterus.
Genetic disorders can also play a role in infertility. Certain genetic conditions can affect reproductive health, making it more difficult for couples to conceive naturally. Genetic testing may be recommended to identify any underlying genetic factors that may be contributing to infertility.
Age-related decline in fertility is a common factor in both men and women. As individuals age, the quality and quantity of eggs and sperm decrease, making it more challenging to conceive. Women are particularly affected by age-related decline in fertility, as their reproductive window is more limited compared to men.
Lifestyle choices can also impact fertility. Smoking, excessive alcohol consumption, drug use, and obesity can all have a negative impact on reproductive health for both men and women. Making healthy lifestyle choices can improve fertility outcomes and increase the chances of successful conception.
Understanding the common causes of infertility in both men and women is crucial in developing a comprehensive treatment plan. By identifying the underlying factors contributing to infertility, healthcare providers can recommend appropriate interventions and assist couples in their journey towards parenthood.
The Journey of Infertility Treatment

Infertility can be a challenging and emotional journey for couples who are longing to start a family. Fortunately, advancements in medical science have provided various treatment options and procedures to help couples overcome infertility. Let’s take a closer look at the stages involved in the journey of infertility treatment.
Initial Consultation and Diagnosis
When a couple decides to seek medical assistance for infertility, the first step is to schedule an initial consultation with a fertility specialist. This consultation is a crucial starting point, as it allows the specialist to gather important information about the couple’s medical history and assess their fertility potential.
During the initial consultation, the fertility specialist will take the time to listen to the couple’s concerns and answer any questions they may have. The specialist will also conduct a thorough physical examination of both partners to identify any underlying health issues that may be contributing to infertility.
In addition to the physical examination, the couple will undergo a series of diagnostic tests. These tests may include blood work to evaluate hormone levels, imaging procedures such as ultrasounds to assess the reproductive organs, and semen analysis to evaluate the male partner’s sperm quality.
Based on the results of these tests, the fertility specialist will provide a diagnosis and explain the potential causes of infertility. This diagnosis is a crucial step in developing a personalized treatment plan that addresses the specific needs of the couple.
Treatment Options and Procedures
Once the couple has received a diagnosis, the fertility specialist will discuss the available treatment options. The choice of treatment will depend on the underlying cause of infertility, the couple’s preferences, and their overall health.
One common treatment option is the use of fertility medications. These medications can help regulate hormonal imbalances, stimulate ovulation in women, or improve sperm production in men. Fertility medications are often the first line of treatment for couples with mild fertility issues.
In some cases, surgical interventions may be necessary to correct anatomical abnormalities that are affecting fertility. These procedures can range from minimally invasive surgeries to more complex operations, depending on the specific condition that needs to be addressed.
For couples who require more advanced interventions, assisted reproductive technologies (ART) offer hope. ART includes procedures such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI). These techniques involve fertilizing eggs outside the body and transferring the resulting embryos into the woman’s uterus.
In certain situations, when the couple is unable to conceive using their own gametes, donor gametes may be considered. Donor eggs or sperm can be used in conjunction with ART to increase the chances of successful pregnancy.
It’s important to note that each treatment option comes with its own set of considerations, including financial costs, potential side effects, and success rates. The fertility specialist will guide the couple through these factors, helping them make informed decisions about their treatment plan.
Throughout the entire journey of infertility treatment, emotional support and counseling play a crucial role. Dealing with infertility can be emotionally draining, and having a support system in place can help couples navigate the ups and downs of the process.
Remember, the journey of infertility treatment is unique to each couple. While it may be challenging at times, it’s important to stay positive and hopeful, knowing that advancements in medical science have made it possible for many couples to fulfill their dreams of parenthood.
Breaking Down the Costs of Infertility Treatment
Understanding the financial implications of infertility treatment is a vital aspect of planning. It is important to note that costs can vary significantly depending on factors such as geographic location, individual insurance coverage, and specific treatment requirements.
Infertility is a complex issue that affects millions of couples worldwide. It can be a challenging and emotional journey, and the financial aspect adds another layer of stress. However, with proper knowledge and planning, individuals can navigate the costs associated with infertility treatment.
Cost of Diagnostic Tests
Diagnostic tests play a fundamental role in identifying the root causes of infertility. These tests can include blood work, ultrasounds, genetic screening, and specialized procedures like hysterosalpingograms. The cost of these tests can range from a few hundred to a few thousand dollars, depending on the complexity and the number of tests required.
It is important to consult with a reproductive endocrinologist or fertility specialist to determine which diagnostic tests are necessary. These tests can provide valuable insights into the underlying causes of infertility, helping healthcare professionals develop an effective treatment plan tailored to each individual’s needs.
Cost of Medications and Supplements
Fertility medications, such as oral or injectable hormones, are often prescribed to stimulate ovulation or enhance sperm production. The cost of these medications can vary significantly depending on the type, dosage, duration of treatment, and any associated side effects.
Some insurance plans may cover a portion of these costs, while others may require individuals to pay out-of-pocket. It is crucial to review insurance coverage carefully and understand the limitations and restrictions regarding fertility medications. Additionally, some pharmaceutical companies offer financial assistance programs or discounts for certain medications, which can help alleviate the financial burden.
Cost of Assisted Reproductive Technologies
Assisted reproductive technologies, such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI), involve more complex procedures that often come with higher costs. These treatments typically involve laboratory procedures, including egg retrieval, sperm processing, and embryo transfer.
The costs associated with ART can include facility fees, medication, laboratory services, anesthesia, and embryo cryopreservation. On average, the cost of a single IVF cycle can range from $12,000 to $15,000, excluding additional expenses for medications or supplementary services.
It is important to note that the success rates of ART can vary depending on various factors, including age, underlying fertility issues, and the quality of embryos. Therefore, individuals may require multiple cycles of treatment, further increasing the overall costs.
Financial planning for infertility treatment is essential. It is advisable to explore various financing options, such as personal savings, loans, or fertility financing programs. Some clinics may offer payment plans or packages that can help individuals manage the costs more effectively.
Additionally, it is crucial to communicate with insurance providers to understand the coverage and reimbursement options available. Some insurance plans may provide partial or full coverage for certain infertility treatments, while others may have specific exclusions or limitations.
Infertility can be a challenging and emotionally draining experience, but with proper financial planning and support, individuals can navigate the costs associated with treatment. It is important to seek guidance from healthcare professionals, financial advisors, and support groups to ensure a comprehensive approach to both the medical and financial aspects of infertility treatment.
Factors Influencing the Cost of Infertility Treatment
Beyond the specific treatment options, several additional factors can influence the overall cost of infertility treatment, including insurance coverage, geographic location, and individual health conditions.
The Role of Insurance in Infertility Treatment
Insurance coverage for infertility treatment varies widely. While an increasing number of insurance plans offer partial or full coverage for certain diagnostic tests or medications, coverage for more advanced treatments such as IVF can be limited or nonexistent. It is crucial to review individual insurance policies and consult with insurance providers to understand coverage limitations and potential out-of-pocket expenses.
Geographic Location and Cost Variation
Costs for infertility treatment can vary significantly depending on the geographical location. Urban areas or regions with higher demand for fertility services generally have a higher cost of living, thus increasing treatment costs. It is essential to research multiple clinics and compare prices, success rates, and services offered to determine the most suitable option.
The Impact of Age and Health Conditions on Treatment Cost
Advanced maternal age and certain health conditions may require additional interventions or higher doses of medications, which can contribute to increased treatment costs. Additionally, couples with complicating factors such as fibroids, endometriosis, or male factor infertility may require additional procedures or surgical interventions, further increasing the overall expense.
Financial Assistance and Support for Infertility Treatment
Recognizing the substantial financial burden associated with infertility treatment, several financial assistance options and support resources are available to couples seeking to build their families.
Grants and Scholarships for Infertility Treatment
Various organizations and foundations offer grants and scholarships to assist couples with the financial burden of infertility treatment. These grants may cover specific treatment procedures, medications, or even the entire cost of a treatment cycle. Researching and applying for such grants can provide much-needed financial support on the fertility journey.
Non-Profit Organizations and Support Groups
Non-profit organizations and support groups dedicated to infertility offer valuable resources, emotional support, and fundraising opportunities. These groups provide guidance on navigating the financial aspects of infertility treatment and facilitate connections with other individuals experiencing similar challenges.
Embarking on the path of infertility treatment requires both emotional and financial strength. By understanding the different factors influencing costs, exploring available financial assistance options, and seeking support, couples can make informed decisions that help fulfill their dreams of starting a family.