Discover the ideal Clomid dosage for men to enhance fertility and address hormonal imbalances.
The Proper Clomid Dosage for Men
Clomid, also known as clomiphene citrate, is a medication that is commonly used in the treatment of fertility issues in women. However, it is also gaining popularity as a treatment option for men. In this article, we will explore the proper Clomid dosage for men, its uses, potential side effects, and monitoring treatment effectiveness.

Understanding Clomid and Its Uses
Clomid is a selective estrogen receptor modulator (SERM) that works by blocking estrogen receptors in the hypothalamus. This stimulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are essential for the production of testosterone and sperm in men.
The Role of Clomid in Men’s Health
Clomid plays a crucial role in men’s health by helping to restore normal testosterone levels. Low testosterone levels can lead to a variety of symptoms, including decreased libido, erectile dysfunction, muscle loss, and fatigue. By increasing testosterone production, Clomid can improve these symptoms and enhance overall well-being.
How Clomid Works in the Body
When Clomid is taken, it binds to estrogen receptors in the hypothalamus, preventing estrogen from exerting its inhibitory effects. This leads to an increase in FSH and LH release, which stimulates the testes to produce more testosterone.
Clomid also has anti-estrogenic effects in other tissues, such as the breast, which can be beneficial for men who are susceptible to estrogen-related side effects from testosterone replacement therapy.
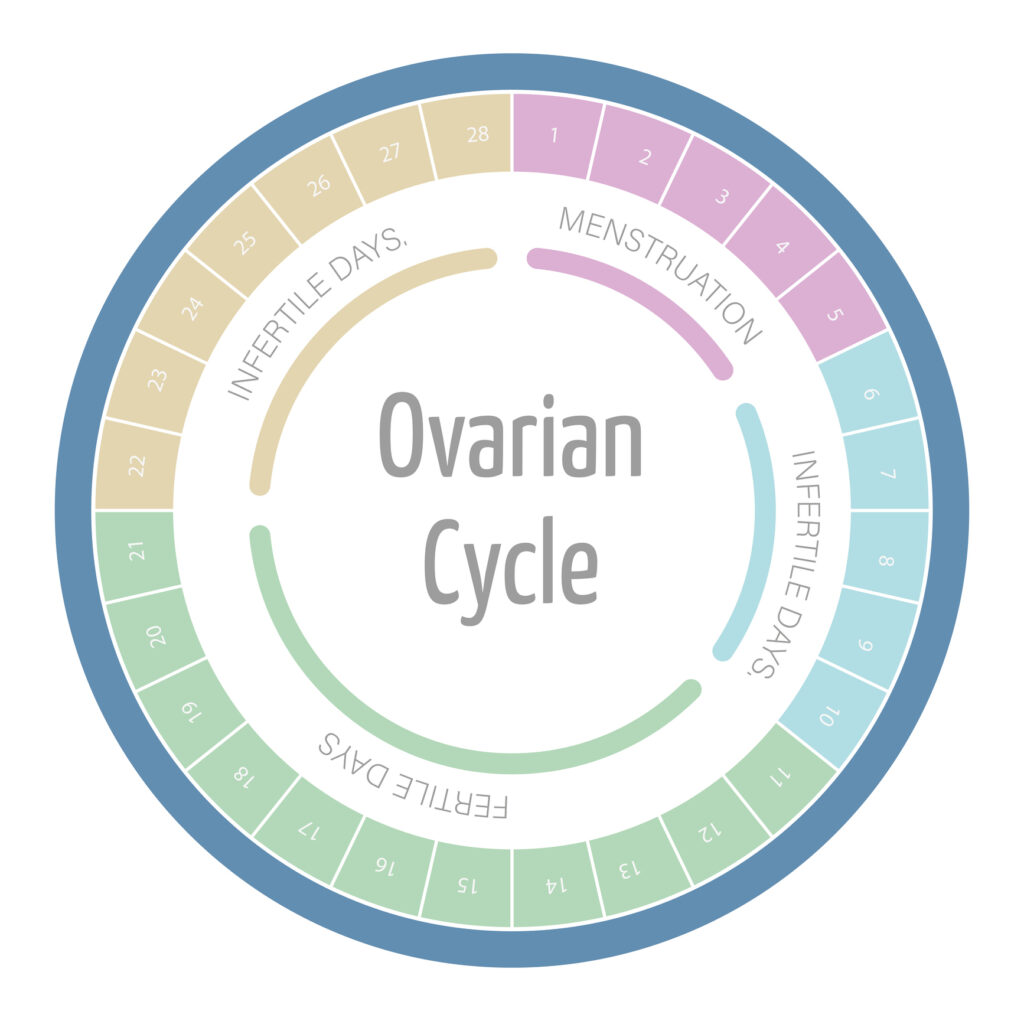
It is important to note that Clomid is not only used in men but also in women. In women, Clomid is commonly prescribed to treat infertility by inducing ovulation. By stimulating the release of FSH and LH, Clomid can help regulate the menstrual cycle and improve the chances of conception.
Potential Side Effects of Clomid
While Clomid is generally well-tolerated, it can cause some side effects in both men and women. Common side effects in men include hot flashes, mood swings, and breast tenderness. In women, side effects may include hot flashes, abdominal discomfort, and changes in cervical mucus.
Determining the Right Dosage
Finding the appropriate Clomid dosage for men can be challenging, as it can vary depending on individual factors. It is important to work closely with a healthcare provider who is experienced in men’s health to determine the right dosage for you.
When considering the dosage of Clomid for men, it’s crucial to understand that this medication is commonly used off-label for treating infertility and low testosterone levels. The dosage prescribed will depend on various factors, such as the underlying cause of the testosterone deficiency and the individual’s response to the treatment.
Factors Influencing Clomid Dosage
Several factors can influence the Clomid dosage for men, including age, weight, medical history, and the severity of testosterone deficiency. A healthcare provider will assess these factors and prescribe the most suitable dosage for each individual.
In addition to the physical factors that influence Clomid dosage, lifestyle choices such as diet, exercise, and smoking habits can also play a role in determining the most effective dosage for men. It’s essential to provide your healthcare provider with a comprehensive overview of your health and lifestyle to ensure the dosage is tailored to your specific needs.
Adjusting Dosage Over Time
The initial Clomid dosage for men is typically low and gradually increased over time. This allows the body to adjust and minimize the risk of side effects. Regular blood tests will be conducted to monitor testosterone levels and make dosage adjustments as needed.
It’s important to note that the effectiveness of Clomid treatment may vary among individuals, and dosage adjustments may be necessary to achieve the desired results. Open communication with your healthcare provider is key to ensuring that the Clomid dosage is optimized for your unique circumstances.
Potential Side Effects of Clomid in Men
While Clomid is generally well-tolerated, there are potential side effects that men should be aware of. It is important to understand the possible outcomes of using this medication for various health conditions.
Clomid, also known as clomiphene citrate, is commonly prescribed to men with infertility issues or hormonal imbalances. This medication works by stimulating the production of hormones that are essential for sperm production and overall reproductive health.
Common Side Effects
Some common side effects of Clomid include hot flashes, mood swings, nausea, headaches, blurred vision, and fatigue. These side effects are usually mild and transient, but it is important to report any concerning symptoms to your healthcare provider. It is crucial to monitor your body’s response to the medication and communicate any changes to your healthcare team for proper management.
Serious Side Effects and When to Seek Help
Although rare, serious side effects of Clomid can occur. These may include visual disturbances, chest pain, shortness of breath, and severe mood changes. If you experience any of these symptoms, it is crucial to seek medical help immediately. Your healthcare provider will be able to assess the severity of the side effects and provide appropriate guidance on the next steps to take.
Additionally, it is essential to follow the prescribed dosage and schedule for Clomid to minimize the risk of adverse effects. Adhering to your healthcare provider’s instructions can help optimize the benefits of the medication while reducing the likelihood of experiencing severe side effects.
Monitoring Treatment Effectiveness
Regular monitoring of treatment effectiveness is essential to ensure optimal results and adjust the Clomid dosage if needed.
When undergoing Clomid treatment, it is crucial to understand the importance of regular monitoring to track progress and make informed decisions regarding dosage adjustments. Healthcare providers will closely monitor your response to the medication through a series of check-ups and blood tests. These assessments allow for the evaluation of testosterone levels and overall treatment effectiveness, enabling healthcare professionals to tailor the dosage to meet your specific needs.
Regular Check-ups and Dosage Adjustments
During the course of Clomid treatment, regular check-ups and blood tests will be conducted to monitor testosterone levels and assess treatment effectiveness. This allows healthcare providers to make necessary dosage adjustments to ensure the best outcomes.
Furthermore, these check-ups provide an opportunity for open communication between you and your healthcare team. By sharing any concerns or observations regarding your response to Clomid, you contribute valuable insights that can guide treatment decisions. Your active participation in this monitoring process is key to optimizing the effectiveness of the medication.
Signs of Improvement and Success
Signs of improvement and success while taking Clomid may include increased libido, improved erectile function, increased muscle mass, and elevated energy levels. It is important to communicate these positive changes to your healthcare provider for ongoing evaluation of treatment effectiveness.
Moreover, recognizing and acknowledging these positive changes is not only beneficial for tracking progress but also serves as motivation throughout your treatment journey. Your healthcare provider will consider these improvements alongside clinical data to ensure that your Clomid dosage remains appropriate and effective.
Frequently Asked Questions About Clomid Dosage
Here are some commonly asked questions about Clomid dosage in men:

Can Clomid Dosage be Increased?
In some cases, the Clomid dosage may need to be increased if the initial dosage is not effective in restoring testosterone levels. This decision will be made by your healthcare provider based on ongoing monitoring and evaluation.
It’s important to note that increasing the Clomid dosage should only be done under the supervision of a healthcare professional. Regular monitoring of hormone levels and potential side effects is crucial to ensure the safe and effective use of Clomid in men.
What Happens if a Dose is Missed?
If a dose of Clomid is missed, it is important to take it as soon as you remember. However, if it is close to the time for the next dose, it is best to skip the missed dose and continue with the regular dosing schedule. It is important not to double the dose to make up for a missed one.
Consistency in taking Clomid as prescribed is key to maintaining stable hormone levels and maximizing the benefits of treatment. Missing a dose occasionally may not have a significant impact, but it’s essential to strive for adherence to the recommended dosing schedule for optimal results.
Overall, the proper Clomid dosage for men is crucial in achieving optimal treatment results. Working closely with a knowledgeable healthcare provider will help ensure the appropriate dosage, regular monitoring, and adjustments as needed to enhance men’s health and well-being.
Remember, individual responses to Clomid dosage can vary, so open communication with your healthcare provider about any concerns or changes in symptoms is essential for personalized care and treatment success.