Discover the ultimate guide to finding the optimal Clomid dosage for boosting male testosterone levels.
Optimal Clomid Dosage for Male Testosterone: A Comprehensive Guide
Clomid is a medication that is commonly used in the treatment of infertility in women. However, it is also gaining popularity as a treatment for low testosterone levels in men. In this comprehensive guide, we will delve into the science behind Clomid, explore its role in testosterone production, discuss the factors influencing Clomid dosage, and highlight the potential side effects of this medication. Additionally, we will outline the importance of monitoring testosterone levels while on Clomid and answer some frequently asked questions about Clomid dosage. So, let’s dive in and learn more about the optimal Clomid dosage for male testosterone.
Understanding Clomid and Its Role in Testosterone Production
Before delving into the optimal Clomid dosage, it is essential to understand how Clomid affects testosterone levels in men. Clomid, also known as clomiphene citrate, belongs to a class of medications called selective estrogen receptor modulators (SERMs). It works by increasing the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in the body, which in turn stimulates the testes to produce more testosterone.
The Science Behind Clomid
Clomid acts on the hypothalamus, a region of the brain that regulates the production of FSH and LH. It binds to estrogen receptors in the hypothalamus and blocks their action, leading to an increase in the release of gonadotropin-releasing hormone (GnRH). This, in turn, stimulates the pituitary gland to release more FSH and LH, resulting in an increase in testosterone production.
How Clomid Affects Testosterone Levels
By increasing the production of FSH and LH, Clomid helps to stimulate the Leydig cells in the testes, which are responsible for testosterone production. This increase in testosterone levels can have a positive impact on various aspects of male health, including libido, energy levels, muscle mass, and overall well-being.
It is important to note that Clomid is primarily used in men with hypogonadism, a condition where the body does not produce enough testosterone, leading to symptoms such as fatigue, decreased libido, and infertility. Clomid is often prescribed off-label for men who are experiencing suboptimal testosterone levels but do not meet the criteria for hypogonadism.
When considering Clomid therapy, it is crucial to work closely with a healthcare provider to determine the appropriate dosage and monitoring schedule. Regular blood tests are typically conducted to assess testosterone levels and adjust the dosage as needed to achieve optimal results while minimizing potential side effects.
Determining the Optimal Dosage of Clomid for Men
The optimal dosage of Clomid for men is a critical aspect of hormone therapy that requires careful consideration of various factors. These factors include the individual’s age, medical history, and baseline testosterone levels. Consulting with a knowledgeable healthcare professional who specializes in hormone therapy is essential to ensure that the dosage is tailored to meet your specific needs and optimize treatment outcomes.
When embarking on Clomid therapy, it is crucial to understand the factors that influence dosage determination. Healthcare professionals take into account the severity of testosterone deficiency, the patient’s weight, and any underlying medical conditions that may impact treatment efficacy. A comprehensive evaluation is necessary to establish a personalized treatment plan that addresses your unique requirements and health status.
Factors Influencing Clomid Dosage
Factors such as the individual’s response to treatment, changes in testosterone levels, and symptom improvement play a significant role in dosage adjustment. Regular monitoring and assessment are key components of the dosage determination process, allowing healthcare professionals to make informed decisions and optimize treatment outcomes.
It’s important to note that while Clomid can be highly effective in treating testosterone deficiency, prolonged use without breaks can potentially lead to desensitization of the hypothalamus-pituitary-testicular axis. To mitigate this risk, healthcare providers often recommend periodic breaks from Clomid therapy to maintain the balance of hormonal regulation.
The Process of Dosage Determination
Initiating Clomid therapy typically involves starting with an initial dosage of 25-50 mg per day, with adjustments made based on individual response and treatment goals. The gradual titration of dosage aims to achieve the optimal balance of testosterone levels while minimizing potential side effects. Collaborating closely with your healthcare provider throughout the treatment process is essential to ensure that the dosage is adjusted as needed to support your overall health and well-being.
Potential Side Effects of Clomid in Men
While Clomid is generally well-tolerated, like any medication, it can have side effects. It’s important to be aware of these potential side effects and discuss them with your healthcare professional before starting Clomid therapy.
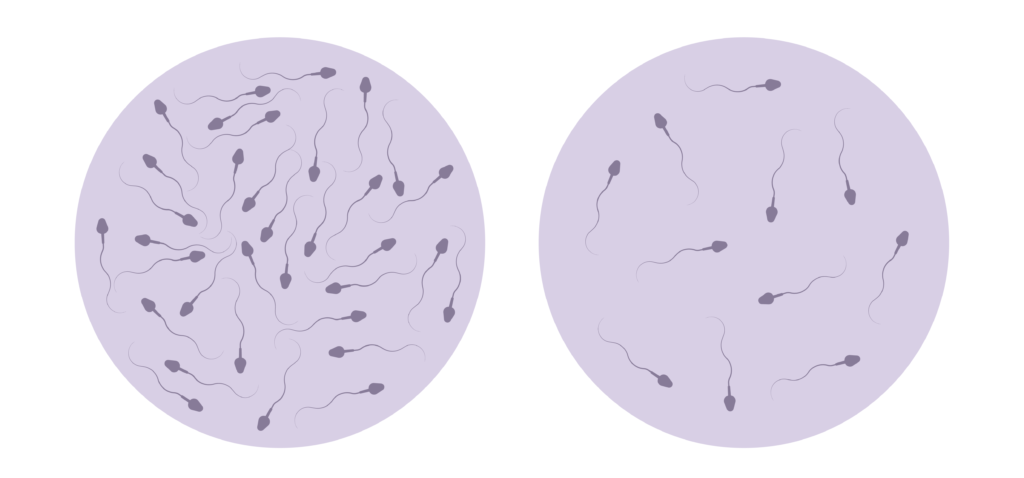
Clomid, also known as clomiphene citrate, is commonly prescribed to men with low testosterone levels or infertility issues. It works by stimulating the production of hormones necessary for sperm production and testosterone levels. However, like all medications, Clomid can have both common and rare side effects that users should be aware of.
Common Side Effects
The most common side effects of Clomid in men include hot flashes, mood swings, fatigue, headaches, and temporary visual disturbances. These side effects are usually mild and tend to diminish as the body adjusts to the medication. It’s important to note that not all individuals will experience these side effects, and they may vary in intensity from person to person.
Another common side effect of Clomid in men is an increase in the size of the testicles. This is due to the stimulation of hormone production and is typically a temporary effect. While it may cause discomfort for some individuals, it is generally not a cause for concern and should subside once the treatment is completed.
Serious Side Effects and Risks
In rare cases, Clomid can cause more severe side effects, such as blurred vision, severe abdominal pain, shortness of breath, and chest discomfort. These symptoms may indicate a serious reaction to the medication and require immediate medical attention. It’s crucial to report any unusual or concerning side effects to your healthcare provider promptly.
Monitoring Testosterone Levels While on Clomid
Regular monitoring of testosterone levels is crucial while undergoing Clomid therapy. This helps healthcare professionals gauge the effectiveness of the treatment and make necessary adjustments to the dosage if needed.
The Importance of Regular Monitoring
By monitoring testosterone levels, healthcare professionals can ensure that the dosage of Clomid is optimized to achieve the desired therapeutic effect. This also helps in identifying any potential side effects or fluctuations in hormone levels promptly.
Understanding Testosterone Level Readings
Testosterone levels are typically measured through a blood test. The normal range for testosterone levels in men varies depending on age, but a healthy range is generally considered to be between 300 and 1,000 nanograms per deciliter (ng/dL). Regular blood tests allow healthcare professionals to track changes in testosterone levels and adjust the Clomid dosage accordingly.
It is important to note that testosterone levels can fluctuate throughout the day, with the highest levels usually seen in the morning. For this reason, healthcare providers often recommend that blood tests for testosterone levels be conducted in the morning for more accurate results.
Factors Affecting Testosterone Levels
Various factors can influence testosterone levels, including age, overall health, and lifestyle choices. Chronic stress, lack of sleep, poor diet, and certain medical conditions can all contribute to fluctuations in testosterone levels. Monitoring these levels regularly can help healthcare professionals identify any underlying issues that may be affecting testosterone production.
Frequently Asked Questions About Clomid Dosage
Can Clomid Dosage Be Adjusted Over Time?
Yes, Clomid dosage can be adjusted over time. Depending on the individual’s response to treatment, healthcare professionals may increase or decrease the dosage to achieve optimal testosterone levels. Regular monitoring helps guide dosage adjustments to ensure the desired therapeutic effect.
It’s important to note that the adjustment of Clomid dosage should always be done under the supervision of a healthcare provider. Monitoring hormone levels and overall health is crucial in determining the effectiveness of the treatment. Changes in dosage may be necessary to address any side effects or to enhance the benefits of Clomid therapy.
What to Do If You Miss a Dose?
If you miss a dose of Clomid, it’s important not to double the dose to make up for the missed one. Simply take the next scheduled dose as prescribed. If you have any concerns or questions about missed doses, it’s best to consult with your healthcare professional for guidance.
Consistency in taking Clomid as prescribed is key to achieving the desired results. Missing a dose occasionally may not have a significant impact, but it’s essential to maintain a regular dosing schedule to optimize the treatment’s effectiveness. Your healthcare provider can provide personalized advice on how to handle missed doses and keep you on track with your Clomid therapy.
Overall, finding the optimal Clomid dosage for male testosterone requires careful evaluation and monitoring by a healthcare professional. With the right dosage, Clomid can help restore testosterone levels and improve various aspects of male health. However, it’s crucial to follow medical advice and discuss any concerns or questions with your healthcare professional throughout the treatment process.