Discover the potential benefits and side effects of using Clomiphene Citrate 50 mg for male health.

Understanding Clomiphene Citrate
Clomiphene Citrate is a medication that is commonly used in the treatment of female infertility. However, it is also gaining popularity as a treatment option for men who are experiencing hormone imbalances or fertility issues. In this article, we will explore what Clomiphene Citrate is, how it works, and its various benefits and side effects.
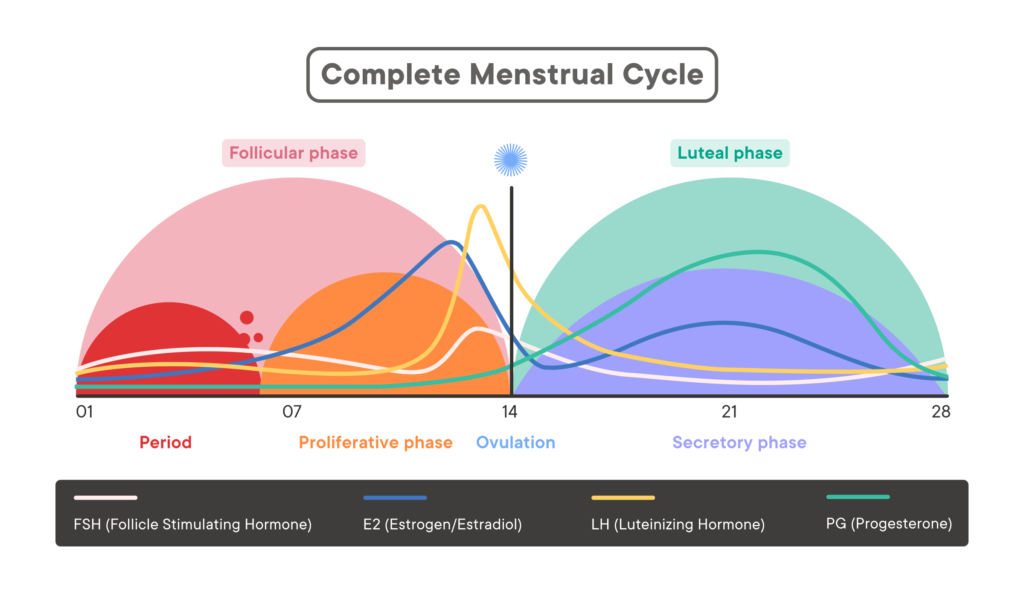
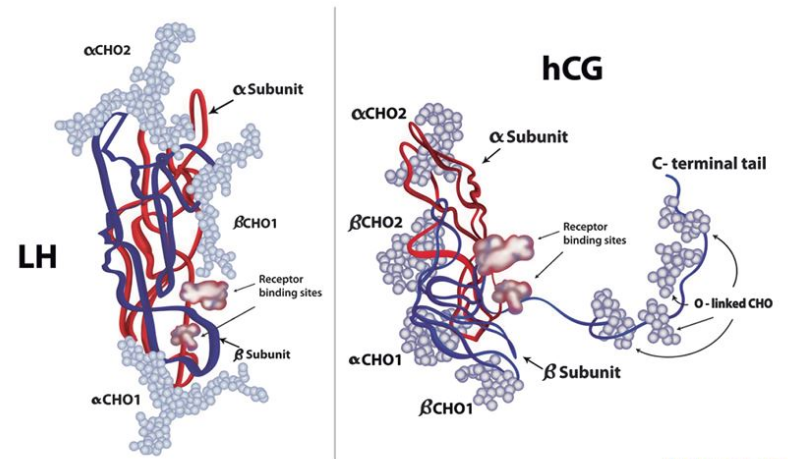
Clomiphene Citrate, also known by its brand name Clomid, is a selective estrogen receptor modulator (SERM). It works by blocking estrogen receptors in the hypothalamus, which leads to an increase in the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These hormones play a crucial role in the regulation of testosterone production in the body.
Clomiphene Citrate works by stimulating the release of hormones that are essential for the production of testosterone. By blocking estrogen receptors, it helps to increase the levels of FSH and LH, which in turn stimulate the testes to produce more testosterone. This increase in testosterone levels can have several positive effects on male health and fertility.
Clomiphene Citrate is often prescribed to men who have low testosterone levels, a condition known as hypogonadism. Low testosterone levels can lead to a variety of symptoms, including fatigue, decreased libido, and erectile dysfunction. By boosting testosterone production, Clomiphene Citrate can help alleviate these symptoms and improve overall quality of life.
Benefits of Clomiphene Citrate for Men
Clomiphene Citrate offers several benefits for men, particularly those who have low testosterone levels or are struggling with fertility issues. Let’s take a closer look at some of its key benefits:
Boosting Testosterone Levels
One of the primary benefits of Clomiphene Citrate is its ability to increase testosterone levels in men. Testosterone is a hormone that is responsible for various aspects of male health, including muscle mass, bone density, sexual function, and mood. By stimulating the production of testosterone, Clomiphene Citrate can help to alleviate the symptoms associated with low testosterone levels.
Improving Fertility
Clomiphene Citrate has been shown to be an effective treatment option for men with fertility issues. By increasing the production of FSH and LH, it helps to stimulate sperm production and improve sperm quality. This can greatly enhance a man’s chances of fathering a child and provide hope for couples struggling with infertility.
Other Potential Health Benefits
In addition to its effects on testosterone and fertility, Clomiphene Citrate has also been reported to have other potential health benefits. Some studies have suggested that it may help to improve cognitive function, increase energy levels, and promote overall well-being. However, further research is needed to fully understand the extent of these potential benefits.
Moreover, Clomiphene Citrate is sometimes used off-label to treat hypogonadism in men. Hypogonadism is a condition where the body doesn’t produce enough testosterone, leading to symptoms such as fatigue, decreased libido, and depression. By stimulating the testes to produce more testosterone, Clomiphene Citrate can help alleviate these symptoms and improve overall quality of life for men with hypogonadism.
It’s important to note that while Clomiphene Citrate can offer significant benefits for men, it may also come with potential side effects. Common side effects may include hot flashes, mood swings, and headaches. It’s crucial for individuals considering Clomiphene Citrate treatment to consult with a healthcare provider to discuss the potential risks and benefits based on their individual health needs.
Side Effects of Clomiphene Citrate in Men
While Clomiphene Citrate offers numerous benefits, it is important to be aware of its potential side effects. Like any medication, Clomiphene Citrate can cause adverse reactions in some individuals. Let’s take a closer look at the possible side effects:
Clomiphene Citrate, commonly used in men for boosting testosterone levels and treating infertility, can sometimes lead to a variety of side effects. It’s crucial for individuals considering this medication to understand both the common and rare side effects that may occur.
Common Side Effects
Common side effects of Clomiphene Citrate in men may include hot flashes, mood swings, nausea, headaches, and blurred vision. These side effects are usually mild and temporary, but if they persist or worsen, it is important to consult a healthcare professional.
Hot flashes, a sudden feeling of warmth spreading through the body, are one of the most reported side effects of Clomiphene Citrate. While they can be bothersome, they are generally not a cause for concern and tend to decrease over time as the body adjusts to the medication.
Serious Side Effects
While rare, Clomiphene Citrate can also cause more serious side effects. These may include abdominal pain, chest pain, shortness of breath, visual disturbances, and allergic reactions. If any of these symptoms occur, immediate medical attention should be sought.
Visual disturbances, such as blurred or double vision, are potential serious side effects of Clomiphene Citrate that require prompt medical evaluation. These symptoms could indicate a more severe underlying issue that needs to be addressed by a healthcare provider.
Long-Term Side Effects
Long-term use of Clomiphene Citrate in men has not been extensively studied, and therefore, the potential long-term side effects are not well known. It is important to discuss any concerns with a healthcare professional and weigh the potential risks against the benefits before starting Clomiphene Citrate treatment.
Individuals considering long-term use of Clomiphene Citrate should be aware that more research is needed to fully understand the effects of prolonged exposure to this medication. Consulting with a healthcare provider regularly can help monitor for any emerging long-term side effects and adjust treatment plans accordingly.
Precautions and Considerations
Before considering Clomiphene Citrate treatment, there are some important precautions and considerations to keep in mind:
Who Should Avoid Clomiphene Citrate?
Clomiphene Citrate is not suitable for everyone. It should be avoided by individuals with a history of liver disease, hormone-related cancers, blood clotting disorders, or allergic reactions to the medication. It is essential to discuss your medical history with a healthcare professional before starting Clomiphene Citrate treatment.
Interactions with Other Medications
Clomiphene Citrate may interact with certain medications, including herbal supplements and over-the-counter drugs. It is important to inform your healthcare provider about all the medications you are currently taking to avoid any potential interactions.
Lifestyle and Dietary Considerations
In addition to medication, maintaining a healthy lifestyle is crucial for overall well-being and optimizing the benefits of Clomiphene Citrate. Regular exercise, a balanced diet, and avoiding smoking and excessive alcohol consumption can all contribute to better health outcomes.
Furthermore, it is worth noting that stress management techniques, such as meditation or engaging in hobbies, can also play a significant role in supporting the effectiveness of Clomiphene Citrate treatment. Stress can have a negative impact on hormone levels and fertility, so finding healthy ways to manage stress can be beneficial.
Moreover, it is important to consider the impact of environmental factors on hormone balance. Exposure to certain chemicals, such as pesticides or endocrine-disrupting substances, can interfere with the body’s hormonal system. Taking steps to minimize exposure to these substances, such as choosing organic produce or using natural cleaning products, can help support the effectiveness of Clomiphene Citrate treatment.
In conclusion, Clomiphene Citrate 50 mg can be a beneficial treatment option for men experiencing hormone imbalances or fertility issues. It offers potential benefits such as boosting testosterone levels, improving fertility, and potentially enhancing overall well-being. However, it is essential to be aware of the possible side effects and take necessary precautions. Consult with a healthcare professional to determine if Clomiphene Citrate is suitable for your specific needs and to ensure safe and effective treatment.