Natural ways of supporting reproductive health
Starting a family can be a beautiful and exciting journey, but for some couples, it’s not always a walk in the park. With modern lifestyles and dietary habits, infertility issues have become more common than ever. Fertility supplements have emerged as a popular and natural way to support reproductive health and improve the chances of conception. In this comprehensive article, we’ll dive deep into the world of fertility supplements and boosting your fertility naturally, answering your burning questions and providing valuable insights to help you make informed decisions.

Fertility Supplements: An Overview
Fertility supplements are a class of nutritional products specifically designed to support and enhance fertility in both men and women. They often contain a blend of vitamins, minerals, herbs, and other natural ingredients that have been scientifically proven to improve reproductive health. In this section, we’ll explore the different types of supplements and their key ingredients.
The Science Behind Fertility Supplements
Fertility supplements work by providing the body with essential nutrients that support hormone balance, egg and sperm health, and overall reproductive function. Some of the key ingredients in supplements include:
- Folic Acid: Crucial for DNA synthesis and cell division, folic acid supports embryo development and helps prevent birth defects.
- Vitamin D: This fat-soluble vitamin is essential for hormone production, immune function, and overall fertility.
- Coenzyme Q10 (CoQ10): An antioxidant that protects cells from damage and supports energy production, CoQ10 is vital for egg and sperm health.
- Omega-3 Fatty Acids: These essential fats help reduce inflammation, support hormone balance, and improve overall reproductive function.
- L-arginine: An amino acid that increases blood flow to the reproductive organs, L-arginine supports healthy egg and sperm production.
Choosing the Right Fertility Supplements
With so many options available, it can be a daunting task to select the right fertility supplements for you and your partner. In this section, we’ll discuss the factors to consider when choosing supplements and provide some tips for finding the best products.
Quality Matters
When shopping for fertility supplements, always prioritize products that are made from high-quality, natural ingredients. Look for supplements that have been independently tested for purity and potency, and avoid products with artificial additives or unnecessary fillers.
Read the Labels
Pay close attention to the ingredient list on the label of the supplements. Ensure they contain the essential nutrients mentioned earlier and avoid products that contain harmful ingredients or allergens.
Consult with a Healthcare Professional
Before starting any supplement regimen, it’s always a good idea to consult with a healthcare professional. They can help you determine the appropriate dosage and recommend specific products based on your unique needs.
Men’s Fertility Supplements
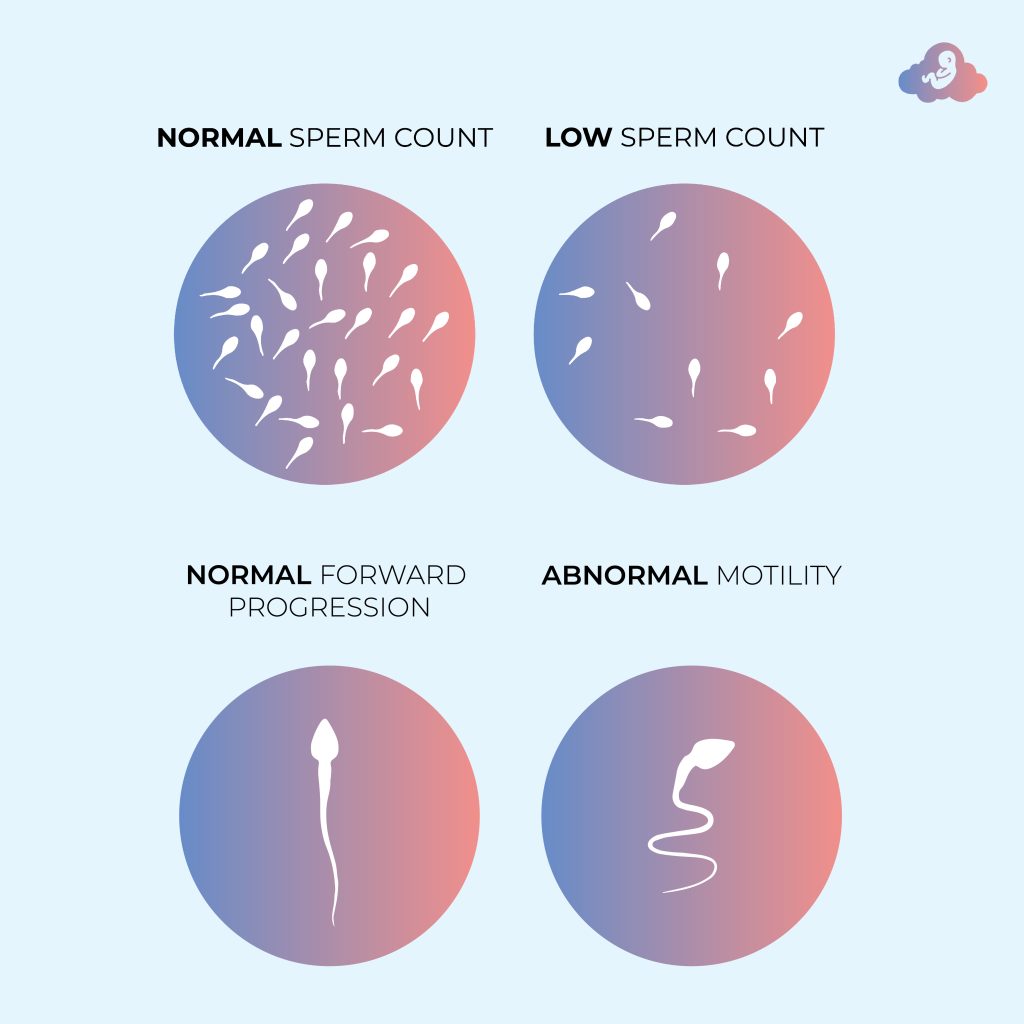
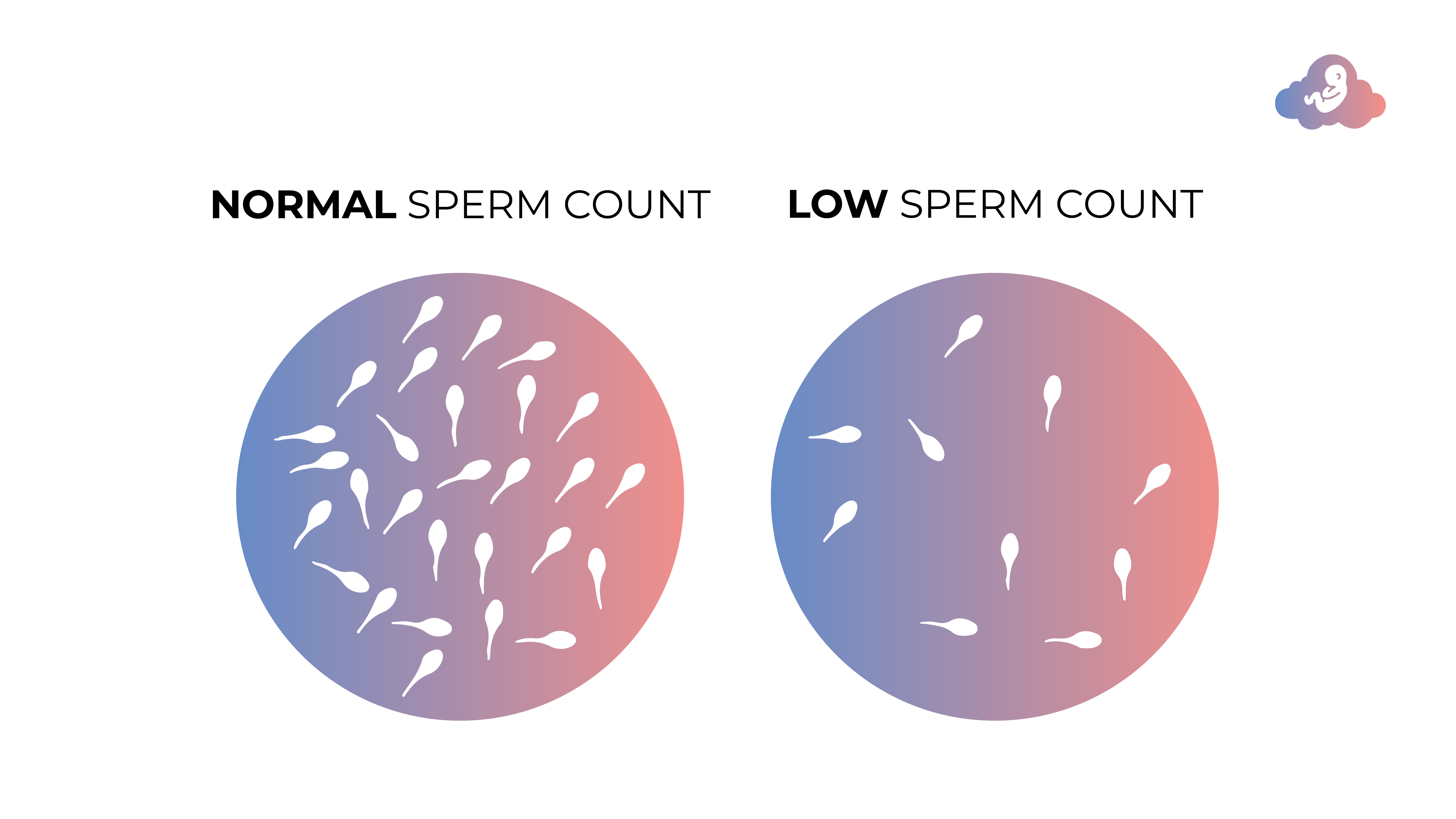
Fertility supplements for men typically focus on supporting sperm health and boosting testosterone levels. Some key ingredients in men’s fertility supplements include:
- Zinc: An essential mineral that supports sperm production and overall male fertility.
- Selenium: This trace mineral plays a crucial role in maintaining healthy sperm motility and function.
- L-carnitine: An amino acid that supports sperm energy production and overall male fertility.
- Maca Root: A Peruvian herb known for its ability to boost libido and improve sperm quality.
Women’s Fertility Supplements
Fertility supplements for women are designed to support hormone balance, improve egg quality, and enhance overall reproductive health. Some key ingredients in women’s fertility supplements include:
- Vitex: A popular herbal remedy that helps balance female hormones and supports regular menstrual cycles.
- Myo-inositol: A naturally occurring substance that improves insulin sensitivity and promotes healthy ovarian function.
- Evening Primrose Oil: Rich in omega-6 fatty acids, this oil is known to support cervical mucus production and overall female fertility.
- Red Raspberry Leaf: A traditional herbal remedy that tones the uterus and helps prepare the body for pregnancy.
Combining Fertility Supplements with Lifestyle Changes
While fertility supplements can be a valuable addition to your journey towards parenthood, it’s important to remember that they work best when combined with a healthy lifestyle. In this section, we’ll explore some lifestyle changes that can further improve your fertility.
Maintain a Healthy Weight
Being overweight or underweight can negatively impact your fertility. Strive to maintain a healthy weight through a balanced diet and regular exercise.
Manage Stress
Chronic stress can wreak havoc on your hormones and reproductive health. Find effective ways to manage stress, such as yoga, meditation, or counseling.
Limit Alcohol and Caffeine Intake
Excessive consumption of alcohol and caffeine can impair fertility. Consider reducing your intake or eliminating these substances altogether.
Quit Smoking
Smoking has been linked to a myriad of fertility issues in both men and women. If you’re a smoker, quitting can significantly improve your chances of conception.
Other ways to Improve your chances naturally
Frequently Asked Questions
Q: How long should I take fertility supplements before trying to conceive?
A: It’s generally recommended to start taking fertility supplements at least three months before trying to conceive. This allows time for the nutrients to accumulate in your body and improve your overall reproductive health.
Q: Are there any side effects associated with fertility supplements?
A: Most fertility supplements are made from natural ingredients and are generally safe to use. However, some individuals may experience mild side effects, such as digestive upset or allergic reactions. If you experience any adverse effects, discontinue use and consult your healthcare provider.
Q: Can I take fertility supplements while undergoing fertility treatments?
A: In many cases, supplements can be safely combined with fertility treatments like IVF or IUI. However, it’s essential to consult with your healthcare provider before taking any supplements during treatment.
Q: Do fertility supplements guarantee pregnancy?
A: While supplements can improve your overall reproductive health and increase your chances of conception, they do not guarantee pregnancy. It’s important to maintain realistic expectations and work closely with your healthcare provider throughout your fertility journey.
Q: Are fertility supplements safe for long-term use?
A: Most fertility supplements are safe for long-term use, but it’s always a good idea to consult with a healthcare professional before starting any supplement regimen. They can help you determine the appropriate duration of use based on your specific needs.
Q: Can I take fertility supplements while pregnant or breastfeeding?
A: Some supplements may be safe to use during pregnancy or breastfeeding, while others may not be recommended. Always consult with a healthcare professional before taking any supplements during pregnancy or while nursing.
Conclusion
Fertility supplements can be a valuable tool in supporting your reproductive health and improving your chances of conception. By understanding the science behind these products, selecting high-quality options, and incorporating healthy lifestyle changes, you can enhance your fertility journey and increase your odds of starting a family. Always consult with a healthcare professional before beginning any supplement regimen and maintain open communication throughout your journey.
To speak with our fertility specialist from the convenience of your home