Explore the connection between C-sections and the onset of endometriosis in this insightful article.
Endometriosis is a complex condition that affects many individuals worldwide, often causing pain and discomfort. For those who have undergone a cesarean section (C-section), concerns about the potential development of endometriosis may arise. This article will delve into the nuances of endometriosis, particularly in the context of women who have had a C-section.
Understanding Endometriosis: What You Need to Know
Endometriosis occurs when tissue similar to the lining inside the uterus, known as the endometrium, grows outside the uterus. This can affect the ovaries, fallopian tubes, and the tissue lining the pelvis. In rare cases, endometrial-like tissue may spread beyond the pelvic organs.

According to the Endometriosis Foundation of America, approximately 1 in 10 women of reproductive age suffers from endometriosis. This can lead to significant pain and complications, including infertility. The exact cause of endometriosis is still under research. With theories ranging from genetic predispositions to hormonal factors and immune system disorders.
Symptoms of endometriosis can vary widely among individuals and may include chronic pelvic pain, painful periods (dysmenorrhea), pain during intercourse, and heavy menstrual bleeding. Additionally, some women may experience gastrointestinal issues such as bloating, diarrhea, or constipation, particularly during their menstrual cycle. The severity of symptoms does not always correlate with the extent of the disease. Some women with mild endometriosis may have severe symptoms, while others with advanced stages may have mild symptoms.
Diagnosis of endometriosis can be challenging, as its symptoms often mimic those of other conditions, such as pelvic inflammatory disease or irritable bowel syndrome. Healthcare providers may conduct a thorough medical history review, pelvic exams, and imaging tests like ultrasounds or MRIs. In some cases, a laparoscopic surgery may be necessary for a definitive diagnosis. This allows doctors to visualize and potentially biopsy the endometrial-like tissue. Early diagnosis and treatment are crucial to managing symptoms and improving quality of life for those affected.
The Link Between C-Sections and Endometriosis: A Closer Look
The relationship between C-sections and the risk of developing endometriosis is a topic of ongoing research. Some studies suggest that surgical procedures such as C-sections could potentially influence the risk. The theory is that surgical trauma may lead to an inflammatory response in the pelvic area. This could promote the growth of endometrial-like tissue inappropriately.
Research published in reputable medical journals indicates mixed results regarding whether there is an increased risk of endometriosis following a C-section. For instance, a study in the journal “Fertility and Sterility” highlighted that women with a history of C-sections might face particular risks associated with pelvic adhesions, which could impact future health, including endometriosis. However, more rigorous and long-term studies are needed to establish a clear link.
Additionally, the hormonal environment post-C-section may also play a role in the development of endometriosis. After a C-section, women experience significant hormonal fluctuations as their bodies adjust to postpartum changes. Some researchers speculate that these hormonal shifts could potentially trigger or exacerbate endometrial-like tissue growth, particularly in women who may already have a predisposition to endometriosis. This connection emphasizes the importance of understanding individual health histories and the potential long-term implications of surgical interventions on reproductive health.
Symptoms of Endometriosis: How to Recognize Them
Recognizing the symptoms of endometriosis is critical for early diagnosis and management. Common symptoms include:
- Painful periods (dysmenorrhea)
- Pelvic pain that may occur before and during menstruation
- Pain during intercourse
- Pain with bowel movements or urination
- Excessive bleeding, particularly during periods
- Infertility issues
The severity of the symptoms is not always indicative of the extent of the condition; some women may experience severe symptoms with minimal endometriosis, while others may have significant endometrial growth with mild symptoms. It’s important to consult with a healthcare provider if these symptoms are experienced, particularly after having a C-section.
In addition to the more commonly recognized symptoms, many women with endometriosis also report experiencing fatigue, gastrointestinal issues such as bloating or nausea, and even psychological symptoms like anxiety and depression. These additional symptoms can significantly impact a woman’s quality of life, making it essential to address them holistically. The chronic pain associated with endometriosis can lead to a cycle of discomfort and emotional distress, which may further complicate the diagnosis and treatment process.
Another important aspect to consider is the variability in symptom presentation among individuals. Some may find that their symptoms fluctuate with hormonal changes, such as during ovulation or when starting or stopping hormonal contraceptives. This variability can sometimes lead to misdiagnosis or delays in receiving appropriate care. Keeping a symptom diary can be a helpful tool for women to track their experiences and provide valuable information to their healthcare providers, ultimately aiding in a more accurate diagnosis and tailored treatment plan.
Risk Factors: Who is Most Likely to Develop Endometriosis?
Several factors can increase a woman’s likelihood of developing endometriosis. These include:
- Age: Particularly between the ages of 25 and 40.
- Family history: Having a family history of endometriosis increases risk.
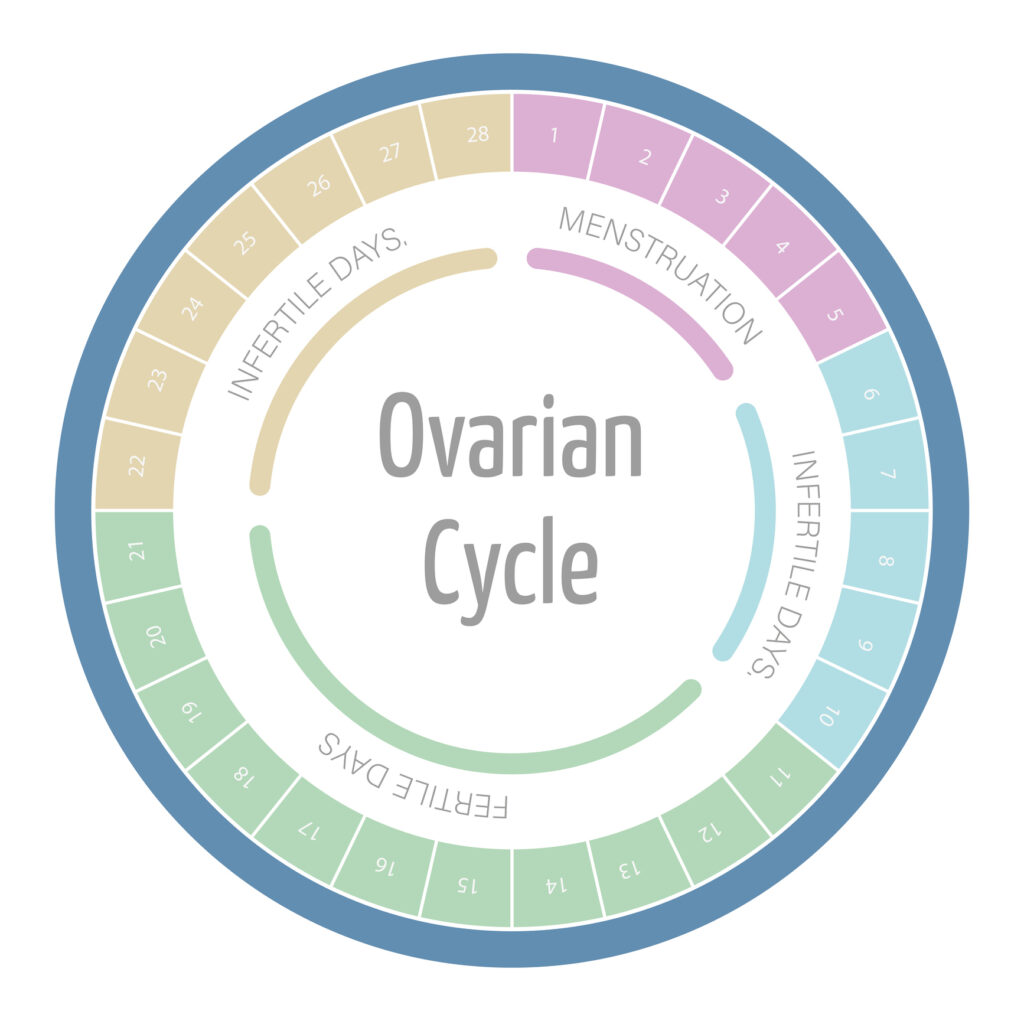
- Menstrual cycle: Short menstrual cycles (less than 27 days) and heavy menstrual flow are linked to endometriosis.
- Medical conditions: Certain conditions such as uterine abnormalities can also increase risk.
- Previous surgeries: Previous surgeries within the pelvic region may elevate the risk.
While researchers continue to explore the potential role of C-sections in endometriosis risk, the consensus remains that multiple factors, including these risk factors, interact to affect overall risk.
Additionally, lifestyle factors may also play a significant role in the development of endometriosis. For instance, women who are overweight or obese may have a higher risk due to the influence of excess body fat on hormone levels, which can exacerbate the symptoms of endometriosis. Furthermore, dietary choices, such as high consumption of red meat and low intake of fruits and vegetables, have been associated with increased risk. These lifestyle elements can contribute to inflammation in the body, potentially worsening the condition.
Moreover, environmental factors are gaining attention in the study of endometriosis. Exposure to certain chemicals and toxins, such as dioxins and polychlorinated biphenyls (PCBs), has been linked to hormonal disruptions that may promote the development of endometriosis. As more research unfolds, understanding the interplay between genetics, lifestyle, and environmental exposures will be crucial in identifying at-risk populations and developing preventive strategies.
Diagnosis: How is Endometriosis Detected After a C-Section?
Diagnosing endometriosis typically involves a combination of patient history, physical examinations, and diagnostic imaging. A healthcare provider may begin with:

- A pelvic exam to feel for cysts or scars behind the uterus.
- Ultrasound imaging to identify any ovarian endometriomas.
- MRI to get a detailed view of the pelvic organs.
In some cases, a laparoscopy may be warranted, which is a surgical procedure that allows direct visualization of the pelvic organs. During this procedure, a doctor may biopsy tissue to confirm the presence of endometrial-like tissue.
For women who have had C-sections, understanding the recovery process and any lingering pelvic pain can be crucial. It is essential to discuss any concerns with a healthcare provider who can guide them through appropriate diagnostic tests. The relationship between C-sections and endometriosis is an area of ongoing research, as some studies suggest that the surgical procedure may inadvertently contribute to the development of endometrial lesions due to changes in the pelvic environment. This makes it even more important for women to be vigilant about their symptoms and seek timely medical advice.
Additionally, the symptoms of endometriosis can often be mistaken for other post-operative complications, such as adhesions or scar tissue from the C-section itself. This overlap can lead to delays in diagnosis and treatment, which is why a thorough evaluation is essential. Women may experience a range of symptoms, including chronic pelvic pain, painful periods, and discomfort during intercourse, all of which can significantly impact their quality of life. Awareness of these symptoms and proactive communication with healthcare providers can help ensure that any underlying conditions are identified and managed effectively.
Treatment Options: Managing Endometriosis Symptoms
Managing and treating endometriosis symptoms can vary widely depending on the severity of the condition, the individual’s health, and their personal treatment preferences. Common treatment options include:
- Over-the-counter pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) may help alleviate pain.
- Hormonal therapies: Birth control pills and hormone therapy can help to regulate or eliminate menstruation and reduce pain.
- GnRH agonists: These may reduce estrogen levels, slowing the growth of endometrial tissue.
- Surgery: In severe cases, surgical options may be necessary to remove endometrial tissue or organs affected by endometriosis.
It’s important to involve a healthcare team specializing in endometriosis to ensure a comprehensive approach to treatment. Evidence from health sources, including the American Congress of Obstetricians and Gynecologists, supports the need for individualized treatment plans based on varying symptoms and lifestyle factors.
Lifestyle Changes
In addition to medical treatments, lifestyle modifications can play a significant role in managing endometriosis symptoms. Many individuals find that incorporating regular exercise, a balanced diet rich in anti-inflammatory foods, and stress management techniques, such as yoga or meditation, can help alleviate some discomfort. Research suggests that maintaining a healthy weight and avoiding certain foods, such as those high in trans fats or refined sugars, may also contribute to symptom relief. Furthermore, support groups and counseling can provide emotional assistance. This helps individuals cope with the psychological impact of living with a chronic condition like endometriosis.
Alternative therapies are also gaining traction among those seeking relief from endometriosis symptoms. Acupuncture, for instance, has been reported by some patients to help reduce pain and improve overall well-being. Herbal supplements, such as ginger or turmeric, are often explored for their anti-inflammatory properties. Although it is crucial to consult with a healthcare provider before starting any new regimen. As research continues to evolve, the integration of complementary therapies alongside conventional treatments may offer a more holistic approach to managing endometriosis, allowing individuals to tailor their care to their unique experiences and preferences.
Preventative Measures: Can You Reduce Your Risk?
While it may not be entirely possible to prevent endometriosis, certain measures may reduce the risk. These include:
- Regular exercise: Engaging in physical activity can help regulate hormones and mitigate symptoms.
- Healthy diet: A balanced diet rich in fruits, vegetables, and whole grains may beneficially impact hormone levels.
- Stress management: Techniques such as yoga, meditation, and counseling may help alleviate stress, which can exacerbate symptoms.
Additionally, some evidence suggests that maintaining a healthy weight and monitoring hormonal health through regular medical check-ups can also contribute to overall reproductive health. As more research emerges, understanding the preventive strategies associated with endometriosis will continue to evolve.
In conclusion, while the connection between C-sections and the development of endometriosis is not fully understood, acknowledgment of the symptoms and proactive medical care are essential for anyone experiencing related health issues. If you have concerns about endometriosis after a C-section, consulting a healthcare provider for personalized advice and support is crucial.