Explore the most effective oligospermia treatment options to boost male fertility and enhance the chances of conception.
Oligospermia, a condition characterized by a low sperm count, can greatly affect a man’s fertility and his ability to conceive a child. While the causes of oligospermia can vary, there are several effective treatment options available. Understanding the condition, implementing lifestyle changes, considering medical interventions, and exploring alternative therapies can all contribute to improving sperm count and enhancing fertility.
Understanding Oligospermia
Oligospermia, also known as low sperm count, occurs when a man’s semen contains fewer sperm than normal. Typically, a healthy sperm count is defined as containing more than 15 million sperm per milliliter of semen. Oligospermia can be caused by a variety of factors, including hormonal imbalances, genetic disorders, certain medications, testicular trauma, and lifestyle choices such as smoking and excessive alcohol consumption.
It is essential to understand that oligospermia can have a significant impact on male fertility and the ability to conceive. Men diagnosed with oligospermia may experience challenges in starting a family and may require medical intervention such as assisted reproductive techniques to achieve pregnancy.
Definition and Causes of Oligospermia
Oligospermia is diagnosed when a man’s semen analysis reveals a sperm count below the normal range. In addition to the aforementioned causes, other factors such as obesity, exposure to environmental hazards, and certain medical conditions like infections or autoimmune disorders can contribute to oligospermia. It is crucial for individuals experiencing oligospermia to seek medical advice and explore treatment options to address this condition effectively.
Furthermore, lifestyle modifications such as maintaining a healthy diet, regular exercise, and avoiding exposure to toxins can play a significant role in improving sperm count and overall reproductive health.
Symptoms and Diagnosis of Oligospermia
In most cases, oligospermia does not present any noticeable symptoms. However, infrequent ejaculation or sexual dysfunction may occur in some individuals. A physical examination, semen analysis, and hormone testing are the primary diagnostic tools used to confirm the presence of oligospermia and determine its underlying cause. Early detection and intervention are key in managing oligospermia and improving the chances of successful conception for couples facing fertility issues.
Lifestyle Changes for Oligospermia Treatment
Making certain lifestyle changes can significantly improve sperm count and overall fertility. These changes include adopting a healthy diet, engaging in regular exercise, managing stress levels, and ensuring adequate sleep.
When it comes to improving sperm count and quality, lifestyle modifications play a crucial role. In addition to the commonly known factors such as diet and exercise, other aspects of daily life can also impact sperm health. For instance, maintaining a healthy weight is important, as obesity has been linked to decreased sperm count and motility. By incorporating a combination of nutritious eating habits and regular physical activity, individuals can work towards achieving a healthier weight and potentially enhance their fertility.
Nutritional Recommendations
A balanced diet rich in antioxidants, vitamins, and minerals is essential for optimal sperm production. Foods such as green leafy vegetables, fruits, whole grains, lean proteins, and nuts are known to promote sperm health. Additionally, avoiding processed foods, excessive caffeine, and alcohol can have a positive impact on sperm count.

Including specific nutrients in the diet can also benefit sperm health. For example, foods high in vitamin C, zinc, and selenium have been associated with improved sperm parameters. Incorporating sources of these nutrients, such as citrus fruits, oysters, and brazil nuts, can be a simple yet effective way to support sperm production and function.
Exercise and Oligospermia
Regular physical activity is beneficial for overall health, including sperm health. Engaging in moderate exercise for at least 30 minutes a day can help improve blood flow to the testicles, which in turn can enhance sperm production. However, it’s important to avoid excessive or intense exercise, as it may temporarily decrease sperm count.

Aside from traditional forms of exercise, activities like yoga or tai chi can also be beneficial for men with oligospermia. These mind-body practices not only help reduce stress levels but also contribute to overall well-being, which can indirectly support sperm health. By incorporating a mix of cardiovascular, strength training, and mind-body exercises into their routine, individuals can optimize their fertility potential.
Impact of Stress and Sleep on Sperm Count
High levels of stress and inadequate sleep can negatively affect sperm production. Finding effective stress-management techniques, such as meditation or yoga, can help alleviate stress and improve sperm count. Additionally, maintaining a regular sleep schedule and aiming for seven to eight hours of quality sleep each night is crucial for reproductive health.

Understanding the connection between stress, sleep, and sperm health is essential for men seeking to address oligospermia. Chronic stress can lead to hormonal imbalances that interfere with sperm production, while poor sleep quality can disrupt the body’s natural rhythms, including those involved in reproductive function. By prioritizing stress reduction strategies and establishing healthy sleep habits, individuals can create a supportive environment for optimal sperm production and fertility.
Medical Treatments for Oligospermia
In cases where lifestyle changes alone are not sufficient, medical interventions may be necessary to treat oligospermia. These treatments may include hormonal therapies, surgical procedures, and assisted reproductive technologies.
When it comes to addressing oligospermia, a condition characterized by a low sperm count, hormonal therapies play a crucial role in restoring the delicate balance of hormones that are essential for sperm production. Hormonal imbalances, such as low levels of testosterone or high levels of estrogen, can significantly impact sperm quality and quantity. By utilizing hormonal treatments like gonadotropin injections or testosterone replacement therapy, healthcare providers aim to regulate these hormone levels and stimulate the production of healthy sperm.
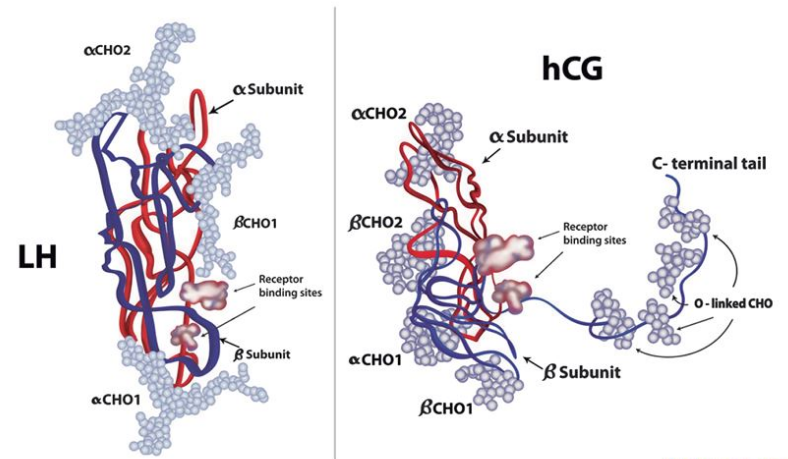
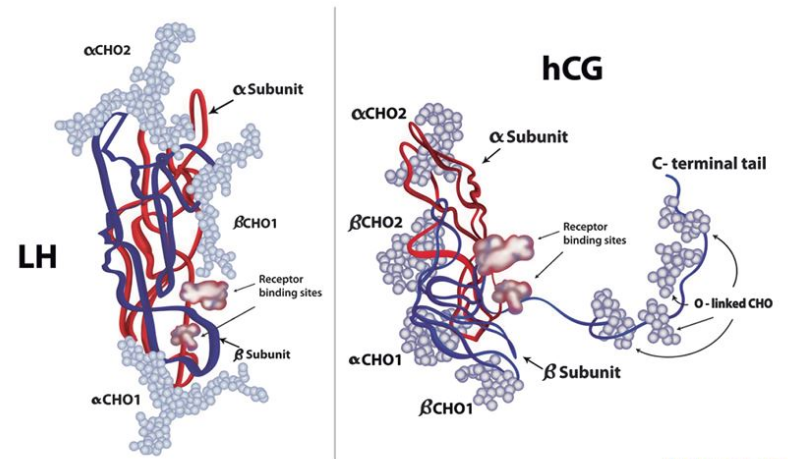
Hormonal Therapies
In some instances, hormonal imbalances may contribute to oligospermia. Hormonal therapies, such as gonadotropin injections or testosterone replacement therapy, can help regulate hormone levels and improve sperm production. However, these treatments should only be administered under the guidance of a healthcare professional.
Moreover, it is crucial to note that hormonal therapies should be carefully monitored to prevent potential side effects and ensure optimal outcomes. Close supervision by medical professionals is essential to adjust dosage levels and assess the individual’s response to treatment, maximizing the chances of success in addressing oligospermia.
Surgical Procedures
Certain structural abnormalities, such as varicoceles or blockages in the reproductive tract, can contribute to oligospermia. Surgical procedures, such as varicocele repair or sperm retrieval techniques, may be recommended to correct these issues and enhance fertility.
When structural issues like varicoceles, which are enlarged veins within the scrotum that can impair sperm production, are identified as contributing factors to oligospermia, surgical intervention becomes a viable treatment option. Varicocele repair surgery aims to improve blood flow and reduce heat buildup in the testicles, creating a more conducive environment for sperm development. Additionally, advanced sperm retrieval techniques, such as testicular sperm extraction (TESE) or microsurgical epididymal sperm aspiration (MESA), can be employed to collect viable sperm directly from the reproductive system for use in assisted reproductive procedures.
Assisted Reproductive Technologies
In cases where other treatments prove ineffective, assisted reproductive technologies (ART) can offer alternative paths to parenthood. Techniques such as intrauterine insemination (IUI) or in vitro fertilization (IVF) can be utilized to maximize the chances of successful conception.
For individuals facing persistent challenges with oligospermia, assisted reproductive technologies present innovative solutions to overcome fertility obstacles. Intrauterine insemination (IUI) involves the direct placement of prepared sperm into the uterus during the woman’s fertile window, increasing the likelihood of successful fertilization. In more complex cases, in vitro fertilization (IVF) offers a comprehensive approach by combining harvested eggs and sperm in a laboratory setting before transferring the resulting embryos into the woman’s uterus. These cutting-edge techniques provide hope for individuals and couples striving to achieve their dream of starting a family despite the complexities of oligospermia.
Alternative Therapies for Oligospermia
In addition to conventional treatments, some individuals explore alternative therapies to complement their oligospermia treatment plan. While the effectiveness of these therapies may vary, they offer potential benefits worth considering.
Herbal Remedies
Certain herbs and supplements, such as maca root, ginseng, or zinc, are believed to enhance sperm count and motility. However, it’s important to consult with a healthcare professional before incorporating any herbal remedies into a treatment regimen, as they may interact with medications or have adverse effects.
Acupuncture and Oligospermia
Acupuncture, an ancient Chinese therapy involving the insertion of thin needles into specific points on the body, has been used to promote fertility. Some studies suggest that acupuncture may improve sperm count and quality by stimulating blood flow to the reproductive organs. However, more research is needed to validate these claims.
Yoga and Meditation for Sperm Health
Practicing yoga and meditation can help reduce stress levels and improve overall well-being, including reproductive health. Certain yoga poses, such as the supported bridge pose or the lotus pose, are believed to stimulate the reproductive organs and enhance sperm production. Incorporating mindfulness and relaxation techniques into daily life can also contribute to improved sperm count.
While alternative therapies can be beneficial, it’s important to approach them with caution and under the guidance of a healthcare professional. It’s crucial to remember that these therapies should not replace conventional medical treatments, but rather be used as complementary approaches to enhance the overall treatment plan.
Another alternative therapy that some individuals explore is the use of traditional Chinese medicine (TCM). TCM practitioners believe that imbalances in the body’s energy, known as qi, can contribute to oligospermia. They may recommend specific herbs, acupuncture, or dietary changes to rebalance the body’s energy and improve sperm health. However, it’s essential to consult with a qualified TCM practitioner who specializes in fertility to ensure safe and effective treatment.
In addition to TCM, some individuals may turn to Ayurvedic medicine, a traditional Indian system of healing. Ayurvedic practitioners focus on balancing the body’s doshas, or energies, to promote overall health and well-being. They may recommend specific herbs, dietary changes, and lifestyle modifications to address oligospermia and improve sperm count. As with any alternative therapy, it’s important to consult with a qualified Ayurvedic practitioner to ensure proper guidance and safe treatment.
It’s worth noting that while alternative therapies can offer potential benefits, they may not work for everyone. Each individual is unique, and what works for one person may not work for another. It’s crucial to approach alternative therapies with an open mind, but also to be realistic about their limitations. Consulting with healthcare professionals and seeking evidence-based information can help individuals make informed decisions about incorporating alternative therapies into their oligospermia treatment plan.