Discover how HCG injections can benefit men’s health in this comprehensive article.
The Benefits of HCG Injections for Men
HCG injections have gained popularity among men seeking various health benefits. This article dives deep into the subject, exploring the role of HCG in the body and how it functions. We will also uncover the science behind HCG injections, highlighting its potential benefits, risks, and frequently asked questions. So, let’s get started on understanding the benefits of HCG injections for men.
Understanding HCG and Its Role in the Body
Before we explore the benefits, let’s understand what HCG is and how it functions in the body.
What is HCG?
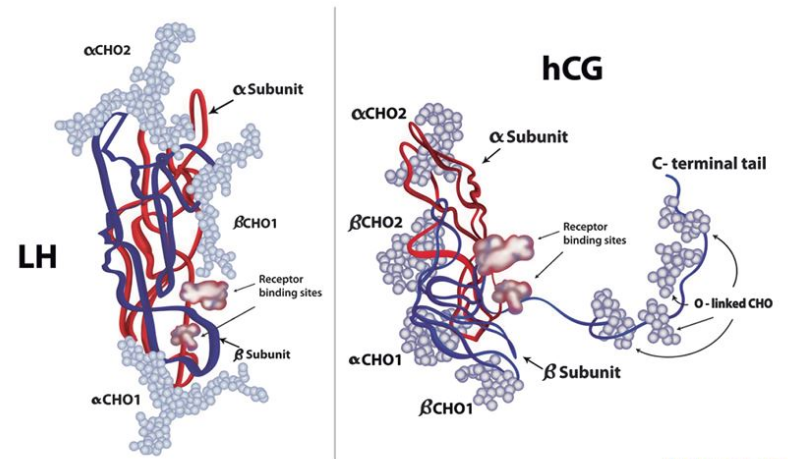
HCG, or human chorionic gonadotropin, is a naturally produced hormone in both men and women. It is primarily associated with pregnancy in women, as it is responsible for maintaining hormonal balance during gestation.
Interestingly, in men, HCG serves a different but equally important purpose. Apart from its role in pregnancy, HCG also aids in stimulating the production of testosterone, the primary male sex hormone. This function is crucial for various bodily functions, including the development of male reproductive tissues and maintaining overall health.
How Does HCG Function in the Body?
Beyond its role in pregnancy, HCG also plays an essential role in the male body. It stimulates the production of testosterone, the primary male sex hormone, which is crucial for various bodily functions.
Now that we have a basic understanding of HCG, let’s take a closer look at how HCG injections work and their impact on the male physiology.
When HCG is administered through injections, it can mimic the action of luteinizing hormone (LH), a hormone that stimulates testosterone production in the testes. This can be particularly beneficial for men with low testosterone levels or those looking to boost their fertility. By increasing testosterone levels, HCG injections can help improve libido, muscle mass, and overall energy levels in men.
The Science Behind HCG Injections for Men
The Process of HCG Injections
HCG injections involve the administration of synthetic HCG into the body. These injections deliver a concentrated dose, bypassing the need for the hormone to be naturally produced.
This method allows for precise control over HCG levels, ensuring consistent and predictable results. For men seeking specific benefits, such as increased testosterone levels, HCG injections can provide a targeted approach.
When considering the process of HCG injections, it’s important to note that this method is often used in conjunction with a specific diet plan, such as the HCG diet. This diet typically involves a low-calorie intake combined with the HCG injections to promote weight loss. The combination is believed to help maintain muscle mass while reducing body fat, leading to a more toned physique.
The Biological Impact of HCG Injections
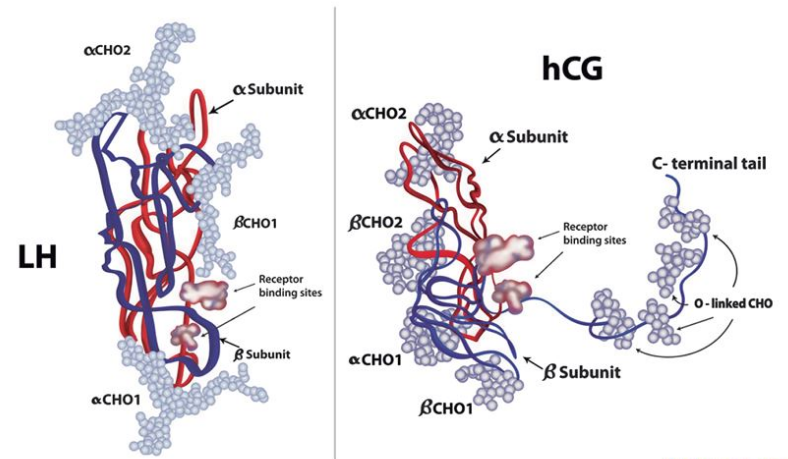
Once injected, HCG stimulates the testes to produce more testosterone. This can lead to various positive effects on men’s health and well-being.
Increased testosterone levels can result in improved energy, enhanced libido, and better mood. They can also contribute to increased muscle mass and strength, making HCG injections appealing to those focused on fitness and bodybuilding.
Furthermore, the impact of HCG injections on fertility is a topic of interest. In some cases, men with low sperm count or other fertility issues may benefit from HCG therapy to stimulate sperm production. This additional benefit of HCG injections showcases the diverse applications of this treatment beyond just testosterone enhancement.
Key Benefits of HCG Injections for Men
Boosting Testosterone Levels
One of the primary benefits of HCG injections for men is the ability to boost testosterone levels. Low testosterone levels can lead to various symptoms such as fatigue, decreased libido, and difficulty gaining muscle mass. HCG injections can help address these concerns and improve overall well-being.
Testosterone is a crucial hormone for men, responsible for regulating sex drive, bone mass, fat distribution, muscle mass and strength, and the production of red blood cells and sperm. By increasing testosterone levels through HCG injections, men may experience improved energy levels, enhanced libido, and better muscle development.
Enhancing Fertility
HCG injections have also been utilized to address male fertility issues. By stimulating testosterone production, HCG can increase sperm count and motility, improving the chances of conception for couples struggling with fertility problems.
Male infertility can be a challenging issue for couples trying to conceive. HCG injections offer a potential solution by supporting the production of healthy sperm, which is essential for successful fertilization. This can bring hope to couples facing difficulties in starting a family.
Weight Loss and Muscle Gain
In addition to its impact on testosterone levels, HCG injections have been associated with weight loss and muscle gain. By increasing metabolism and promoting fat burning, HCG can assist individuals in achieving their weight loss goals. The hormone also helps preserve muscle mass during caloric restriction, making it an attractive option for individuals seeking to improve body composition.
Weight management is a common concern for many individuals, and HCG injections offer a potential solution by boosting metabolism and aiding in fat loss. The preservation of muscle mass is crucial during weight loss efforts to maintain strength and support overall health. Incorporating HCG injections into a comprehensive weight loss plan may help individuals achieve their desired body composition goals.
Potential Side Effects and Risks of HCG Injections
Common Side Effects
While HCG injections offer potential benefits, it is essential to be aware of possible side effects. Common side effects of HCG injections may include injection-site reactions, headache, and mild fluid retention. These side effects are typically temporary and resolve on their own.
It is important to note that individual responses to HCG injections can vary. Some individuals may experience more pronounced side effects, while others may have minimal to no side effects at all. Monitoring your body’s response and communicating any concerns with your healthcare provider is crucial for a safe and effective treatment experience.
Long-Term Risks
Long-term risks associated with HCG injections are still under investigation. Some concerns include the potential impact on natural hormone production and the development of dependency. It is crucial to consult with a medical professional before starting HCG injections.
Research is ongoing to better understand the potential long-term effects of HCG injections on various aspects of health. Studies are exploring the relationship between prolonged HCG use and its effects on metabolic processes, reproductive health, and overall well-being. As with any medical intervention, weighing the benefits against the risks is essential in making informed decisions about your healthcare.
Frequently Asked Questions About HCG Injections
Who Should Consider HCG Injections?
HCG injections are commonly recommended for men dealing with low testosterone levels or fertility issues. Low testosterone can lead to symptoms such as fatigue, decreased muscle mass, and low libido. Fertility issues may arise due to hormonal imbalances affecting sperm production. Consulting with a healthcare professional is crucial to assess your specific situation and determine if HCG injections are a suitable treatment option for you.
It’s important to note that HCG injections are not typically recommended for women, except in certain cases of infertility treatment. Women who are pregnant or breastfeeding should avoid HCG injections due to potential risks to the developing fetus or nursing infant.
How Often Should HCG Injections Be Administered?
The frequency of HCG injections varies based on individual needs and the treatment plan prescribed by a healthcare provider. In some cases, injections may be required once a week, while in others, they may be administered up to three times per week. Regular monitoring by a medical professional is essential to adjust the dosage and frequency of injections as needed to achieve optimal results.
It’s important to follow the recommended injection schedule diligently to maintain consistent hormone levels in the body. Deviating from the prescribed regimen can impact the effectiveness of the treatment and may lead to undesirable side effects.
Can HCG Injections Be Self-Administered?
HCG injections should always be administered under the supervision and guidance of a qualified healthcare professional. Proper injection technique is crucial to ensure the medication is delivered safely and effectively. Healthcare providers can teach patients how to self-administer injections at home, following strict protocols to minimize the risk of infection or injury.
Patient education is key to successful self-administration of HCG injections. Understanding the correct injection site, needle insertion angle, and dosage measurement is essential for a patient to feel confident and comfortable with the process. Any concerns or uncertainties about self-administration should be promptly addressed with the healthcare provider to ensure the safe and proper use of HCG injections.