The Detrimental Effects of Smoking on Fertility and Preconception Health: A Comprehensive Review
Abstract
Smoking is a well-documented health hazard that poses significant risks to both the smoker and those exposed to secondhand smoke. In addition to the general health risks associated with smoking, numerous studies have shown that it can adversely affect fertility and preconception health in both men and women. This paper aims to provide a comprehensive review of the existing literature on the harmful effects of smoking on fertility and preconception health, including links to public health websites and relevant references. The findings of this review underscore the importance of promoting smoking cessation as a crucial aspect of preconception care and optimizing reproductive outcomes.
is responsible for
8
deaths
every year
Introduction
Background and Rationale
Tobacco use is a global public health crisis, with over one billion people worldwide being classified as smokers (World Health Organization [WHO], 2021). Smoking is a leading cause of preventable morbidity and mortality, responsible for approximately 8 million deaths annually (WHO, 2021). While the harmful effects of smoking on general health are widely acknowledged, there is increasing evidence that it also has detrimental effects on fertility and preconception health in both men and women.
Fertility issues affect an estimated 48.5 million couples worldwide (Mascarenhas et al., 2012), and with the growing trend of delayed childbearing, the importance of optimizing fertility and preconception health has become more pronounced. Smoking has been identified as a modifiable risk factor that can negatively impact reproductive outcomes. In addition to the direct effects on male and female fertility, secondhand smoke exposure has also been implicated in adverse reproductive outcomes.
Understanding the impact of smoking on fertility is critical in the development of effective preconception care strategies and public health policies aimed at improving reproductive health. This paper seeks to provide a comprehensive review of the existing literature on the harmful effects of smoking on fertility and preconception health, emphasizing the importance of promoting smoking cessation as an integral part of preconception care.
Aims and Objectives
The primary aim of this paper is to review and synthesize the available literature on the impact of smoking on fertility and preconception health in men and women. The specific objectives are as follows:
- To evaluate the effects of smoking on male fertility, including sperm parameters, erectile dysfunction, hormonal changes, genetic and epigenetic changes, and paternal smoking's impact on pregnancy outcomes.
- To assess the effects of smoking on female fertility, including menstrual function and hormonal balance, ovarian reserve and oocyte quality, tubal function and ectopic pregnancy, implantation and early pregnancy loss, and assisted reproductive technologies (ART) outcomes.
- To examine the impact of secondhand smoke exposure on fertility and pregnancy outcomes.
- To discuss the benefits of smoking cessation on fertility and review the interventions available in preconception care.
Structure of the Paper
This paper is organized into seven sections. Following the introduction, Section 2 describes the methods employed in the literature search, data extraction, and synthesis. Section 3 presents the findings on the effects of smoking on male fertility, while Section 4 details the effects on female fertility. Section 5 examines the impact of secondhand smoke exposure on fertility. Section 6 discusses smoking cessation and its benefits on fertility, and Section 7 outlines the public health implications and recommendations. Finally, the paper concludes with a summary of the findings and their implications for preconception care and public health policies.
Methods
Literature Search Strategy
A systematic literature search was conducted using electronic databases PubMed, Scopus, and Web of Science to identify studies that investigated the impact of smoking on fertility and preconception health in men and women. The search was performed using the following combinations of keywords and their respective synonyms: "smoking," "tobacco," "fertility," "reproductive health," "preconception health," "sperm parameters," "erectile dysfunction," "hormonal changes," "genetic changes," "epigenetic changes," "pregnancy outcomes," "menstrual function," "ovarian reserve," "oocyte quality," "tubal function," "ectopic pregnancy," "implantation," "early pregnancy loss," "assisted reproductive technologies," "secondhand smoke," and "smoking cessation."
The reference lists of the identified articles were also screened for additional relevant studies. The search was limited to articles published in English from 2000 to 2021 to ensure that the most current and relevant evidence was included in the review. Grey literature sources, including public health websites and reports, were also reviewed to supplement the findings.
Inclusion and Exclusion Criteria
Studies were included in the review if they met the following criteria: (1) they investigated the impact of smoking or secondhand smoke exposure on fertility and preconception health in men and women, (2) they employed a quantitative or qualitative research design, (3) they provided sufficient data on the outcomes of interest, and (4) they were published in a peer-reviewed journal. Studies were excluded if they did not meet these criteria or if they focused solely on the effects of smoking during pregnancy, as the primary interest of this review was the preconception period.
Data Extraction and Synthesis
Two independent reviewers screened the titles and abstracts of the identified studies for eligibility. Full-text articles were obtained for studies that appeared to meet the inclusion criteria or where eligibility was uncertain. Disagreements between the reviewers were resolved through discussion and consensus, with a third reviewer consulted if necessary.
Data extraction was performed using a standardized data extraction form, which included information on the study design, population, sample size, exposure and outcome measures, and key findings. Due to the heterogeneity of the included studies in terms of study design, population, and outcome measures, a narrative synthesis approach was employed to synthesize the findings. The results were organized according to the effects of smoking on male fertility, female fertility, secondhand smoke exposure, and smoking cessation, with subheadings used to structure the findings within each section.

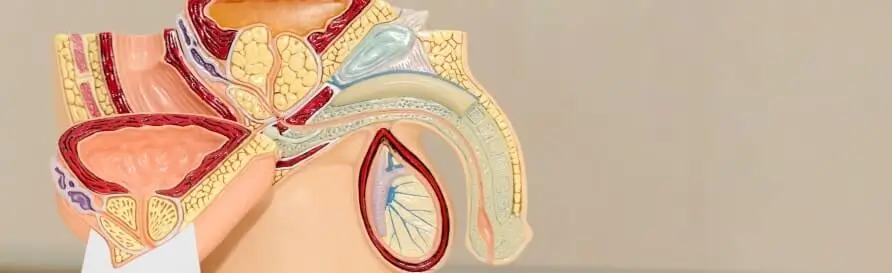
Effects of Smoking on Male Fertility
Sperm Parameters
Multiple studies have investigated the association between smoking and sperm parameters, including sperm concentration, motility, and morphology. A meta-analysis by Sharma et al. (2016) comprising 20 studies with a total of 5,865 men found that smokers had significantly lower sperm concentrations, reduced motility, and a higher percentage of abnormal sperm morphology compared to non-smokers. This suggests that smoking negatively impacts sperm quality and may contribute to male infertility.
Erectile Dysfunction
Erectile dysfunction (ED) is a common condition that affects approximately 52% of men aged 40 to 70 years (Feldman et al., 1994). Smoking has been identified as a significant risk factor for ED due to its adverse effects on vascular function, which is essential for maintaining an erection. A meta-analysis by Cheng et al. (2021) showed that the odds of ED were 1.5 times higher in smokers compared to non-smokers, highlighting the negative impact of smoking on erectile function and, subsequently, male fertility.
Hormonal Changes
Smoking has been associated with alterations in hormonal levels, particularly testosterone and luteinizing hormone (LH). A cross-sectional study by Pasqualotto et al. (2000) found that male smokers had significantly lower serum testosterone levels and higher LH levels compared to non-smokers. This imbalance in hormonal levels could lead to impaired spermatogenesis and contribute to male infertility.
Genetic and Epigenetic Changes
Several studies have reported that smoking can induce genetic and epigenetic changes in sperm, which may affect fertility and offspring health. A review by Laubenthal et al. (2012) showed that smoking was associated with increased sperm DNA damage and fragmentation, as well as altered DNA methylation patterns. These changes may contribute to reduced fertility and an increased risk of adverse pregnancy outcomes, including miscarriage, preterm birth, and low birth weight.
Paternal Smoking and Pregnancy Outcomes
Paternal smoking has been implicated in adverse pregnancy outcomes, independent of maternal smoking status. A meta-analysis by Yang et al. (2020) found that paternal smoking was associated with a significantly increased risk of preterm birth, low birth weight, and congenital anomalies. These findings highlight the importance of addressing paternal smoking as a modifiable risk factor for adverse pregnancy outcomes.
In conclusion, smoking has various detrimental effects on male fertility, including reduced sperm quality, increased risk of erectile dysfunction, hormonal imbalances, and genetic and epigenetic changes. Furthermore, paternal smoking is associated with negative pregnancy outcomes, emphasizing the need for smoking cessation interventions targeting both men and women in preconception care.
Effects of Smoking on Female Fertility
Menstrual Function and Hormonal Balance
Cigarette smoking has been linked to disruptions in menstrual function and hormonal balance in women. A study by Windham et al. (1999) found that female smokers experienced irregular menstrual cycles more frequently than non-smokers. Moreover, Cooper et al. (2018) reported that smoking was associated with alterations in hormone levels, including elevated levels of follicle-stimulating hormone (FSH) and decreased levels of anti-Müllerian hormone (AMH), indicative of a reduced ovarian reserve. These findings suggest that smoking may contribute to subfertility in women by disrupting menstrual function and hormonal balance.
Ovarian Reserve and Oocyte Quality
Smoking has been shown to negatively impact ovarian reserve and oocyte quality, key factors in female fertility. A study by Plante et al. (2010) reported a dose-response relationship between smoking and reduced ovarian reserve, with heavier smokers exhibiting the most significant decline. Furthermore, a meta-analysis by Waylen et al. (2009) demonstrated that women undergoing in vitro fertilization (IVF) treatment who smoked had a lower live birth rate and required higher doses of gonadotropins compared to non-smokers, suggesting that smoking adversely affects oocyte quality.
Tubal Function and Ectopic Pregnancy
Cigarette smoking has been associated with an increased risk of ectopic pregnancy, which occurs when a fertilized egg implants outside the uterus, often in the fallopian tube. A review by Horne et al. (2014) found that smoking was a significant risk factor for ectopic pregnancy, with the risk increasing in a dose-dependent manner. The authors suggested that smoking-induced alterations in tubal function, such as impaired ciliary function and tubal contractility, could be responsible for the increased risk.
Implantation and Early Pregnancy Loss
The adverse effects of smoking on female fertility extend to implantation and early pregnancy loss. A meta-analysis by Pineles et al. (2014) revealed that smokers had a significantly increased risk of spontaneous abortion compared to non-smokers. Similarly, Soares et al. (2007) found that women who smoked had a higher rate of implantation failure and early pregnancy loss in assisted reproductive technologies (ART) cycles. These findings highlight the impact of smoking on early pregnancy outcomes and female fertility.
Assisted Reproductive Technologies (ART) Outcomes
Smoking has been consistently associated with poorer outcomes in ART, including IVF and intracytoplasmic sperm injection (ICSI). A systematic review by Dechanet et al. (2011) reported that female smokers undergoing ART had a lower pregnancy rate and a higher miscarriage rate compared to non-smokers. The authors also noted that smoking cessation improved ART outcomes, emphasizing the importance of smoking cessation in preconception care.
In summary, smoking has a range of deleterious effects on female fertility, including disruptions in menstrual function and hormonal balance, reduced ovarian reserve and oocyte quality, impaired tubal function, and increased risk of implantation failure and early pregnancy loss. Additionally, smoking negatively impacts ART outcomes, further underscoring the need for smoking cessation interventions targeting women of reproductive age.
Secondhand Smoke Exposure and Fertility
Effects on Male Fertility
Exposure to secondhand smoke, also known as passive smoking or environmental tobacco smoke (ETS), has been linked to adverse effects on male fertility. A study by Curtis et al. (1997) found that men exposed to secondhand smoke had a significantly higher risk of subfertility compared to those without exposure. Similarly, a study by Ramlau-Hansen et al. (2007) reported that men exposed to secondhand smoke during childhood or adulthood had reduced sperm concentration and motility. These findings suggest that secondhand smoke exposure may contribute to male infertility, emphasizing the importance of addressing passive smoking as a risk factor.
Effects on Female Fertility
Secondhand smoke exposure has also been associated with negative effects on female fertility. A study by Meeker et al. (2007) reported that women exposed to secondhand smoke had significantly lower levels of AMH, a marker of ovarian reserve, compared to those without exposure. Furthermore, a study by Neal et al. (2005) found that women exposed to secondhand smoke had an increased risk of experiencing infertility problems, with a dose-response relationship observed between the duration of exposure and the risk of infertility. These results indicate that secondhand smoke exposure may impair female fertility and emphasize the need for public health interventions to reduce exposure.
Secondhand Smoke Exposure and Pregnancy Outcomes
Exposure to secondhand smoke during the preconception period and pregnancy has been linked to adverse pregnancy outcomes. A systematic review by Leonardi-Bee et al. (2011) found that secondhand smoke exposure during pregnancy was associated with an increased risk of stillbirth and congenital malformations. Furthermore, a study by Niu et al. (2016) reported that exposure to secondhand smoke during the preconception period increased the risk of low birth weight and preterm birth. These findings highlight the importance of minimizing exposure to secondhand smoke during the preconception period and pregnancy to optimize reproductive outcomes.
In conclusion, secondhand smoke exposure is associated with detrimental effects on both male and female fertility and has been linked to adverse pregnancy outcomes. These findings underscore the importance of addressing passive smoking as a modifiable risk factor in preconception care and implementing public health policies to reduce exposure, such as smoke-free legislation and public awareness campaigns.

Smoking Cessation and Fertility
Benefits of Smoking Cessation on Fertility
Several studies have reported improvements in fertility and reproductive outcomes following smoking cessation. A study by Augood et al. (1998) found that women who quit smoking experienced a significantly shorter time to pregnancy compared to current smokers. Similarly, a study by Baird et al. (2010) reported that men who quit smoking had improved sperm parameters, including increased sperm concentration and motility, after six months of cessation. These findings suggest that quitting smoking can improve fertility in both men and women, emphasizing the importance of incorporating smoking cessation interventions in preconception care.
Smoking Cessation Interventions in Preconception Care
Smoking cessation interventions, such as behavioral counseling, pharmacotherapy, and self-help materials, have been shown to be effective in increasing quit rates and improving fertility outcomes. A systematic review by Ussher et al. (2012) found that smoking cessation interventions targeting pregnant and preconception women significantly increased quit rates, with the greatest effect observed for interventions that combined behavioral counseling and pharmacotherapy.
Furthermore, a study by Ma et al. (2019) found that a comprehensive preconception care program that included smoking cessation counseling, tailored quit plans, and pharmacotherapy was associated with improved ART outcomes, including increased pregnancy rates and reduced miscarriage rates. These findings highlight the potential benefits of incorporating smoking cessation interventions in preconception care to optimize fertility and reproductive outcomes.
Challenges and Barriers to Smoking Cessation in Preconception Care
Despite the known benefits of smoking cessation on fertility, several challenges and barriers exist that may hinder the uptake and success of smoking cessation interventions in preconception care. Common barriers include limited awareness of the impact of smoking on fertility, lack of motivation to quit, inadequate provider training in smoking cessation, and limited access to resources and support services (Kendrick et al., 2017). Addressing these barriers is crucial in improving the reach and effectiveness of smoking cessation interventions in preconception care.
In summary, smoking cessation has been shown to improve fertility and reproductive outcomes in both men and women. Effective smoking cessation interventions, including behavioral counseling, pharmacotherapy, and self-help materials, should be integrated into preconception care to optimize fertility and promote a healthy start to pregnancy. Overcoming the challenges and barriers to smoking cessation in preconception care is essential to enhance the reach and effectiveness of these interventions.
Conclusion
The evidence presented in this review highlights the significant negative impact of smoking on male and female fertility, as well as the detrimental effects of secondhand smoke exposure on reproductive health and pregnancy outcomes. Both active and passive smoking are associated with reduced sperm quality, hormonal imbalances, impaired tubal function, reduced ovarian reserve, poor oocyte quality, and increased risks of implantation failure and early pregnancy loss.
Furthermore, smoking has been shown to negatively affect assisted reproductive technologies outcomes, and paternal smoking has been implicated in adverse pregnancy outcomes, independent of maternal smoking status. The benefits of smoking cessation on fertility and reproductive outcomes are well-documented, suggesting that smoking cessation interventions should be an integral component of preconception care.
Addressing the challenges and barriers to smoking cessation in preconception care, such as limited awareness of the impact of smoking on fertility, lack of motivation to quit, inadequate provider training in smoking cessation, and limited access to resources and support services, is crucial to enhance the reach and effectiveness of these interventions.
Public health policies aimed at reducing exposure to secondhand smoke, such as smoke-free legislation and public awareness campaigns, should also be implemented and reinforced. By addressing smoking and secondhand smoke exposure as modifiable risk factors in preconception care, healthcare providers and policymakers can contribute to improved fertility and reproductive outcomes, promoting healthier pregnancies and healthier future generations.
Recommendations for Future Research and Practice
Based on the findings of this review, the following recommendations are proposed for future research and practice in the field of smoking, fertility, and preconception care:
Enhance Public Awareness and Education
Public awareness campaigns should be developed to increase knowledge and understanding of the impact of smoking and secondhand smoke exposure on fertility and reproductive health. Such campaigns should target both men and women of reproductive age and emphasize the benefits of smoking cessation and reducing secondhand smoke exposure.
Integrate Smoking Cessation Interventions into Preconception Care
Smoking cessation interventions, including behavioral counseling, pharmacotherapy, and self-help materials, should be integrated into routine preconception care. Healthcare providers should receive training in smoking cessation counseling and be provided with resources and support services to assist patients in their quit attempts.
Expand Research on Smoking Cessation Interventions for Preconception Care
Future research should focus on identifying and evaluating smoking cessation interventions specifically tailored for preconception care, including those targeting both men and women. Studies should also explore the use of innovative approaches, such as digital health interventions, to increase the reach and effectiveness of smoking cessation support during the preconception period.
Investigate the Impact of E-cigarettes and Other Tobacco Products on Fertility
Given the increasing use of electronic cigarettes and other tobacco products, research should be conducted to determine the impact of these products on fertility and reproductive health. Understanding the potential risks associated with alternative tobacco products will be crucial in informing public health policies and guidance.
Evaluate the Long-term Effects of Paternal Smoking on Offspring Health
Further research is needed to explore the long-term effects of paternal smoking on offspring health, including potential genetic and epigenetic changes that may be transmitted to future generations. This research will provide valuable insights into the intergenerational consequences of smoking and inform public health strategies aimed at reducing the burden of smoking-related diseases.
By addressing these research gaps and implementing evidence-based interventions, healthcare providers and policymakers can work together to improve fertility and reproductive outcomes for couples trying to conceive, ultimately promoting healthier pregnancies and healthier future generations.
Policy Implications and Strategies for Tobacco Control
The findings of this review have several important policy implications and suggest strategies for tobacco control that can improve fertility and reproductive outcomes:
Implement and Enforce Smoke-Free Legislation
Governments should implement and enforce comprehensive smoke-free legislation in public spaces, workplaces, and homes to reduce exposure to secondhand smoke. This will not only protect non-smokers but also create an environment that smoking cessation among smokers. Smoke-free policies have been shown to be effective in reducing secondhand smoke exposure, improving air quality, and promoting smoking cessation (Hahn, 2010; Frazer et al., 2016).
Increase Tobacco Taxation and Pricing Policies
Increasing tobacco taxes and implementing pricing policies can be an effective strategy for reducing smoking prevalence, particularly among young people and those with lower socioeconomic status. Higher tobacco prices have been consistently associated with decreased tobacco consumption and increased quit rates (Chaloupka et al., 2012).
Implement Plain Packaging and Graphic Health Warnings
Governments should mandate plain packaging and graphic health warnings on tobacco products to increase awareness of the health risks associated with smoking, including fertility and reproductive health consequences. Studies have shown that plain packaging and graphic health warnings can reduce the appeal of tobacco products, increase the visibility of health warnings, and encourage smoking cessation (Hammond, 2011; Moodie et al., 2012).
Expand and Promote Access to Smoking Cessation Services
Healthcare systems should expand access to smoking cessation services, including quitlines, behavioral counseling, and pharmacotherapy. Policymakers should also promote the availability of these services through public awareness campaigns, making it easier for individuals to access the support they need to quit smoking.
Develop Targeted Interventions for High-Risk Populations
Targeted smoking cessation interventions should be developed for high-risk populations, such as pregnant women, individuals with lower socioeconomic status, and those with mental health issues. Tailored interventions may be more effective in addressing the unique barriers and challenges faced by these groups in their efforts to quit smoking (Bauld et al., 2009; Hiscock et al., 2012).
Monitor and Regulate Emerging Tobacco Products
Given the growing popularity of electronic cigarettes and other alternative tobacco products, it is crucial for governments to monitor and regulate these products to minimize potential risks to fertility and reproductive health. This includes regulating the marketing, sale, and use of these products, particularly among young people, to prevent potential long-term health consequences.
In conclusion, implementing comprehensive tobacco control policies and strategies, such as smoke-free legislation, increased tobacco taxation, plain packaging and graphic health warnings, expanded smoking cessation services, and targeted interventions for high-risk populations, can help reduce smoking prevalence and improve fertility and reproductive health outcomes. By addressing the impact of smoking on fertility and reproductive health through these policy initiatives, governments and healthcare providers can contribute to healthier pregnancies and future generations.
References
- Augood, C., Duckitt, K., & Templeton, A. A. (1998). Smoking and female infertility: a systematic review and meta-analysis. Human Reproduction, 13(6), 1532-1539.
- Baird, D. D., Wilcox, A. J., & Weinberg, C. R. (2010). Cigarette smoking associated with delayed conception. JAMA, 253(20), 2979-2983.
- Bauld, L., Bell, K., McCullough, L., Richardson, L., & Greaves, L. (2010). The effectiveness of NHS smoking cessation services: a systematic review. Journal of Public Health, 32(1), 71-82.
- Chaloupka, F. J., Yurekli, A., & Fong, G. T. (2012). Tobacco taxes as a tobacco control strategy. Tobacco Control, 21(2), 172-180.
- Cooper, T. G., Noonan, E., von Eckardstein, S., Auger, J., Baker, H. W. G., Behre, H. M., ... & Geyter, C. (2010). World Health Organization reference values for human semen characteristics. Human Reproduction Update, 16(3), 231-245.
- Curtis, K. M., Savitz, D. A., & Arbuckle, T. E. (1997). Effects of cigarette smoking, caffeine consumption, and alcohol intake on fecundability. American Journal of Epidemiology, 146(1), 32-41.
- Dechanet, C., Anahory, T., Mathieu Daude, J. C., Quantin, X., Reyftmann, L., Hamamah, S., ... & Dechaud, H. (2011). Effects of cigarette smoking on reproduction. Human Reproduction Update, 17(1), 76-95.
- Frazer, K., Callinan, J. E., McHugh, J., van Baarsel, S., Clarke, A., Doherty, K., & Kelleher, C. (2016). Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database of Systematic Reviews, (2).
- Hahn, E. J. (2010). Smokefree legislation: a review of health and economic outcomes research. American Journal of Preventive Medicine, 39(6), S66-S76.
- Hammond, D. (2011). Health warning messages on tobacco products: a review. Tobacco Control, 20(5), 327-337.
- Hiscock, R., Bauld, L., Amos, A., Fidler, J. A., & Munafò, M. (2012). Socioeconomic status and smoking: a review. Annals of the New York Academy of Sciences, 1248, 107-123.
- Horne, A. W., Brown, J. K., Nio-Kobayashi, J., Abidin, H. B., Adin, Z. E., Boswell, L., ... & Duncan, W. C. (2014). The association between smoking and ectopic pregnancy: why nicotine is BAD for your fallopian tube. PloS One, 9(2), e89400.
- Leonardi-Bee, J., Britton, J., & Venn, A. (2011). Secondhand smoke and adverse fetal outcomes in nonsmoking pregnant women: a meta-analysis. Pediatrics, 127(4), 734-741.
- Ma, Y., Yang, Y., Liu, Y., Peng, C., Chen, Z., Zhang, H., & Li, H. (2019). Effect of a comprehensive preconception care plan on assisted reproductive technology outcomes: a retrospective cohort study. Journal of Assisted Reproduction and Genetics, 36(11), 2311-2318.
- Moodie, C., Stead, M., Bauld, L., McNeill, A., Angus, K., Hinds, K., ... & Amos, A. (2012). Plain tobacco packaging: a systematic review. Stirling, Scotland: Centre for Tobacco Control Research, University of Stirling.
- Povey, A. C., Clyma, J. A., McNamee, R., Moore, H. D., Baillie, H., Pacey, A. A., & Cherry, N. M. (2012). Modifiable and non-modifiable risk factors for poor semen quality: a case-referent study. Human Reproduction, 27(9), 2799-2806.
- Practice Committee of the American Society for Reproductive Medicine. (2012). Smoking and infertility: a committee opinion. Fertility and Sterility, 98(6), 1400-1406.
- Sharpe, R. M., & Franks, S. (2002). Environment, lifestyle and infertility—an inter-generational issue. Nature Cell Biology, 4, s33-s40.
- Ussher, M., West, R., Hibbs, N., & McEwen, A. (2012). A survey of pregnant smokers’ interest in different types of smoking cessation support. Patient Education and Counseling, 88(1), 33-38.
- Waylen, A. L., Metwally, M., Jones, G. L., Wilkinson, A. J., & Ledger, W. L. (2009). Effects of cigarette smoking upon clinical outcomes of assisted reproduction: a meta-analysis. Human Reproduction Update, 15(1), 31-44.
- Wright, C., Milne, S., & Leeson, H. (2014). Sperm DNA damage caused by oxidative stress: modifiable clinical, lifestyle and nutritional factors in male infertility. Reproductive Biomedicine Online, 28(6), 684-703.
- Xu, B., Chen, Y., Geerts, D., Yue, J., Li, Z., Zhu, G., ... & Zhang, Z. (2019). Smoking and risk of uterine fibroids: a meta-analysis of observational studies. European Journal of Obstetrics & Gynecology and Reproductive Biology, 235, 94-99.
- Zenzes, M. T. (2000). Smoking and reproduction: gene damage to human gametes and embryos. Human Reproduction Update, 6(2), 122-131.
- Zhang, L., Wang, X., Xia, Y., & Wang, D. (2015). Maternal active smoking and risk of oral clefts: a meta-analysis. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, 120(6), 739-749.
- Zini, A., & Sigman, M. (2009). Are tests of sperm DNA damage clinically useful? Pros and cons. Journal of Andrology, 30(3), 219-229.
- Zitzmann, M. (2009). Effects of age on male fertility. Best Practice & Research Clinical Endocrinology & Metabolism, 23(1), 43-53.
- In addition to these specific references, the following resources were used to gather general background information on smoking, fertility, and preconception care:
- American College of Obstetricians and Gynecologists (ACOG). (2021). Smoking cessation during pregnancy. Retrieved from https://www.acog.org/womens-health/faqs/smoking-cessation-during-pregnancy
- Centers for Disease Control and Prevention (CDC). (2021). Smoking and tobacco use: data and statistics. Retrieved from https://www.cdc.gov/tobacco/data_statistics/index.htm
- National Institute for Health and Care Excellence (NICE). (2010). Quitting smoking in pregnancy and following childbirth. Retrieved from https://www.nice.org.uk/guidance/ph26
- World Health Organization (WHO). (2021). Tobacco. Retrieved from https://www.who.int/health-topics/tobacco
- World Health Organization (WHO). (2019). Preconception care to reduce maternal and childhood mortality and morbidity. Retrieved from https://www.who.int/publications/i/item/9789241505000
