The Impact of Alcohol Consumption on Fertility and Preconception Health
Abstract
This research paper investigates the potential harms of alcohol consumption on fertility and preconception health. The growing prevalence of alcohol consumption among those attempting to conceive underscores the urgency of this public health issue. Drawing from a wide range of biochemical, epidemiological, and psychosocial studies, the paper delineates the multifaceted ways in which alcohol can impede conception and compromise fetal health. It delves into the biochemical disruptions caused by alcohol, including hormonal imbalances and degradation of sperm and egg quality, as well as potential genetic risks to the embryo. The paper further scrutinizes epidemiological studies that reveal correlations between alcohol consumption and fertility issues, miscarriage rates, and fetal health complications. It also considers the indirect impacts of alcohol consumption, such as its role in lifestyle factors and mental health conditions that can detrimentally affect fertility. Through the lens of public health, the paper examines current recommendations and the effectiveness of interventions aimed at mitigating the risks associated with alcohol consumption during the preconception period. The findings of this research emphasize the need for ongoing investigation, more comprehensive public health policies, and robust health promotion campaigns to protect and enhance fertility and preconception health.
Introduction
Investigating the Intersection of Alcohol and Reproductive Health
The intersection of alcohol consumption and reproductive health is a crucial area of investigation due to the significant implications for individuals and societies alike. This paper seeks to dissect the potential harms of alcohol consumption on fertility and preconception health.
Alcohol, a psychoactive substance predominantly consumed for its recreational properties, is widely used across the globe. However, its consumption is associated with a range of health issues, from liver disease to mental health disorders. Fertility, defined as the natural capability to produce offspring, and preconception health, which refers to the health of women and men during their reproductive years, are not immune to the deleterious effects of alcohol.
Trends and Concerns: Alcohol Consumption Among Prospective Parents
A disconcerting trend is the widespread prevalence of alcohol consumption among those attempting to conceive. In the United States, for example, approximately 50% of pregnancies are unplanned, and many women might not realize they are pregnant until 4-6 weeks into the pregnancy, potentially exposing the developing fetus to alcohol (CDC, 2020). Furthermore, the normalization of alcohol in social situations can lead to regular consumption during the preconception period, raising concerns about its impact on fertility and the health of the potential offspring.
Aims and Scope of the Study: Uncovering Alcohol's Impacts on Fertility and Preconception Health
The purpose of this research is to elucidate the harmful effects of alcohol on fertility and preconception health. It aims to synthesize evidence from various fields, including biochemical research, epidemiological studies, and psychosocial considerations. By exploring these multiple dimensions, the paper seeks to provide a comprehensive understanding of how alcohol consumption can affect the journey to parenthood.
The significance of this study extends beyond academic interest. The findings have the potential to inform public health policy, shape health promotion campaigns, and guide clinical practice. Ultimately, the goal is to arm individuals and health professionals with the knowledge needed to make informed decisions about alcohol consumption during the preconception period, contributing to healthier pregnancies and healthier future generations.

Literature Review
The detrimental health effects of alcohol are well-documented. However, its specific impact on fertility and preconception health is a subject that warrants further exploration. This literature review seeks to examine the body of existing research in this domain, focusing on studies that investigate the effects of alcohol consumption on reproductive health.
Impact of Alcohol on General Health
Several studies have explored the impact of alcohol on general health. Alcohol consumption is known to contribute to the development of numerous physical and mental health conditions, including cardiovascular diseases, liver diseases, and depression World Health Organization, 2018. The biochemical changes induced by alcohol are believed to interfere with many body functions, which potentially include reproductive functions.
Alcohol's Role in Reproductive Health and Fertility
Moving to research specifically related to reproductive health, alcohol's role appears to be multifaceted and somewhat complex. Several epidemiological studies have suggested a correlation between alcohol consumption and fertility issues. A study by Eggert, Theobald, and Engfeldt (2004) found that women consuming more than 14 alcoholic drinks per week were 50% more likely to report fertility problems than those who consumed less.
A significant body of research has also explored the effects of alcohol on male fertility. A systematic review by Ricci et al. (2017) suggested a detrimental effect of alcohol on semen volume, sperm concentration, and sperm morphology, especially in men consuming at least five drinks per week.
In terms of preconception health, the implications of alcohol consumption extend beyond the individuals trying to conceive. Studies have linked maternal alcohol consumption to a range of complications, including miscarriage, premature birth, low birth weight, and Fetal Alcohol Spectrum Disorders (FASDs) (CDC, 2020). Similarly, paternal alcohol consumption has been associated with an increased risk of congenital malformations (Li et al., 2019).
Identifying Gaps and Future Research Directions
While these studies provide valuable insights, a gap exists in the literature concerning the in-depth investigation of how alcohol affects fertility and preconception health. There are potential biochemical, lifestyle, and societal aspects that may contribute to these effects, and these warrant further investigation. The current study intends to explore these dimensions, synthesizing a comprehensive understanding of the impact of alcohol on fertility and preconception health.
The Biochemical Impact of Alcohol on Reproductive Health
The biochemical processes within the human body are intricate and delicately balanced. Alcohol, with its known ability to disrupt numerous biological functions, can significantly impact reproductive health. This section examines the various ways in which alcohol interferes with the biochemical balance crucial to reproduction.
Alcohol's Influence on Hormonal Balance and Reproductive Health
Alcohol's impact on hormone balance is one of the key factors affecting reproductive health. Alcohol affects the hypothalamic-pituitary-gonadal (HPG) axis, a system of interactions between the hypothalamus, pituitary gland, and gonadal glands responsible for the control of reproductive hormones Mendelson and Mello, 1988. Excessive alcohol consumption can cause irregular menstrual cycles and anovulation in women by inhibiting the secretion of gonadotropin-releasing hormone (GnRH) in the hypothalamus, which in turn affects the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In men, alcohol can reduce testosterone levels while increasing estrogen levels, potentially leading to decreased libido and quality of sperm.
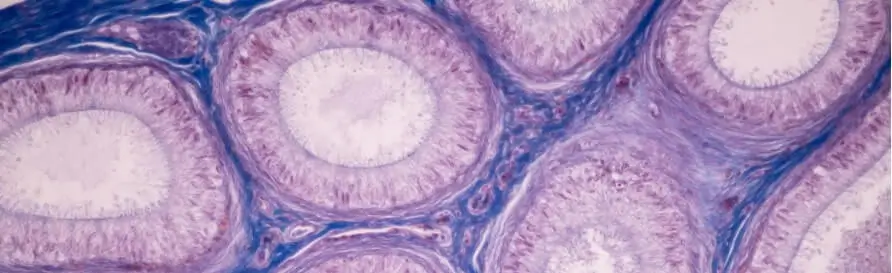
Direct Impact of Alcohol on Sperm and Egg Quality
The direct impact of alcohol on the quality of sperm and eggs is another area of concern. Research by La Vignera et al. (2013) suggests that chronic alcohol abuse can lead to sperm abnormalities, including changes in sperm morphology and decreased motility. Similarly, alcohol can negatively affect oocyte health in women. Animal studies have shown that alcohol exposure can cause abnormalities in the zona pellucida (the outer layer of the egg), potentially reducing the chances of successful fertilization and implantation Kasai et al., 2006.
Alcohol's Genetic Risks to the Embryo
Beyond the impact on the sperm and egg, alcohol can pose genetic risks to the developing embryo. Alcohol metabolites can cause oxidative stress and DNA damage Bailey and Sokol, 2011. This genotoxic stress can lead to mutations and genomic instability in the developing embryo, increasing the risk of birth defects and developmental disorders, including Fetal Alcohol Spectrum Disorders (FASDs).
In conclusion, alcohol's biochemical impact on reproductive health is multifaceted and concerning. By disrupting hormonal balance, degrading the quality of reproductive cells, and posing genetic risks to the embryo, alcohol consumption can significantly undermine fertility and preconception health. This evidence underscores the importance of alcohol abstinence or moderation for those planning to conceive.
The Epidemiological Evidence
Epidemiological studies offer a wealth of data demonstrating correlations between alcohol consumption and various fertility and preconception health issues. This section will review some of these findings, highlighting the impact of alcohol on fertility, miscarriage rates, and fetal health.
Implications of Alcohol on Fertility
A number of studies have suggested a link between alcohol consumption and fertility issues. In a Danish prospective cohort study involving 6,120 women trying to conceive, alcohol consumption of 14 or more servings per week was associated with an 18% decrease in fecundability compared to no alcohol consumption Hakonsen et al., 2016. Another study by Eggert, Theobald, and Engfeldt (2004) found that women consuming more than 14 alcoholic drinks per week were 50% more likely to report fertility problems than those who consumed less.
Increased Miscarriage Rates Associated with Alcohol Consumption
Alcohol consumption has also been associated with increased miscarriage rates. A large cohort study by Andersen et al. (2012) found that consumption of 5 or more alcoholic drinks per week was associated with an increased risk of first trimester miscarriage. This aligns with findings from other studies, such as the one by Rasch (2003), which indicated a 2- to 3-fold increased risk of early miscarriage with the consumption of 5 drinks per week compared to women who did not consume alcohol.
Detrimental Effects of Alcohol on Fetal Health
Finally, numerous studies have shown the adverse effects of alcohol on fetal health. Fetal Alcohol Spectrum Disorders (FASDs) are perhaps the most well-known of these, encompassing a range of physical, cognitive, and behavioral problems in individuals exposed to alcohol in utero. The prevalence of FASDs in the United States is estimated to be as high as 2-5% May et al., 2014. In addition to FASDs, alcohol exposure can lead to other fetal health issues such as low birth weight, preterm birth, and stillbirth Patra et al., 2011.
In conclusion, the epidemiological evidence strongly suggests that alcohol consumption can have detrimental effects on fertility and preconception health, from decreased fertility rates to increased risks of miscarriage and fetal health complications. These findings underscore the importance of public health interventions aimed at reducing alcohol consumption in those planning to conceive.
The Psychological and Lifestyle Factors
Alcohol Consumption and Lifestyle Patterns Negatively Impacting Fertility
While the biochemical and epidemiological impacts of alcohol on reproductive health are significant, it is also essential to consider the psychological and lifestyle factors that can be influenced by alcohol. This section will explore the indirect ways that alcohol can affect fertility and preconception health.
Firstly, alcohol consumption is often integrated into lifestyle patterns that may not be conducive to optimal fertility. For example, heavy drinking is frequently associated with other unhealthy behaviors such as poor diet, lack of physical activity, and smoking, all of which can negatively affect fertility Bolúmar et al., 1997. Moreover, alcohol's role in sexual behavior should not be overlooked. Studies have shown that alcohol can increase the likelihood of risky sexual behavior, leading to higher rates of sexually transmitted infections (STIs), which can further impact fertility Cook and Clark, 2005.
Mental Health Concerns and Societal Norms: The Overlooked Contributors
Alcohol's impact on mental health is another critical factor. Chronic alcohol use is associated with a higher prevalence of mental health disorders, including depression and anxiety Rehm et al., 2003. These conditions can create additional stress, which in turn can affect fertility. Research has shown that stress can lead to irregular menstrual cycles and reduced sperm quality, which can hinder conception Louis et al., 2011.
Finally, societal norms and expectations play a significant role in shaping alcohol consumption habits, which can indirectly impact fertility and preconception health. In many societies, moderate to heavy drinking is normalized or even encouraged in certain social situations. This normalization can mask the potential risks of alcohol to fertility and preconception health, leading to a lack of awareness and increased susceptibility to these risks.
In conclusion, the psychological and lifestyle factors associated with alcohol use can indirectly impact fertility and preconception health. These effects, coupled with the direct biochemical impacts of alcohol, underline the need for a comprehensive approach to alcohol and reproductive health. This approach should encompass not only medical interventions but also psychological support and societal-level changes in attitudes and norms around alcohol consumption.

Case Study: Public Health Interventions
Given the substantial evidence linking alcohol consumption to negative impacts on fertility and preconception health, public health interventions are essential for mitigating these risks. This section examines some of the interventions that have been implemented and their effectiveness.
U.S. Public Health Intervention: CDC's Campaign on FASDs
One notable initiative is the U.S. Centers for Disease Control and Prevention's (CDC) campaign on Fetal Alcohol Spectrum Disorders (FASDs). The campaign, 'Alcohol and Pregnancy: Why Take the Risk?' aims to raise awareness about the risks of alcohol consumption during pregnancy and promote alcohol abstinence for those planning to conceive or who are pregnant CDC, 2020. The campaign uses multiple channels, including social media, television, and healthcare provider toolkits, to reach a broad audience. Although it's challenging to measure the direct impact of such campaigns, they are vital for raising awareness and promoting informed decision-making.
UK's Public Health Approach: NICE Guidelines on Preconception Health
In the United Kingdom, the National Institute for Health and Care Excellence (NICE) has guidelines that advise healthcare professionals to inform women planning a pregnancy about the potential risks of alcohol consumption. The guidelines also recommend offering information and advice about alcohol consumption as part of antenatal care NICE, 2010. These guidelines ensure that women receive consistent information from healthcare professionals about the potential risks of alcohol.
Australian Strategy: NHMRC's Recommendations for Alcohol Abstinence
Lastly, in Australia, the National Health and Medical Research Council (NHMRC) updated their guidelines in 2020 to recommend that "to prevent harm from alcohol to their unborn child, women who are pregnant or planning a pregnancy should not drink alcohol" NHMRC, 2020. The guideline update was widely publicized and has been influential in shaping public opinion and behavior regarding alcohol consumption in the preconception period and pregnancy.
These case studies illustrate the variety of interventions that can be employed to reduce the harmful effects of alcohol on fertility and preconception health. The combination of public awareness campaigns, healthcare professional guidelines, and national health recommendations are all vital tools in this public health effort. However, more research is needed to evaluate the effectiveness of these interventions and to continue developing innovative strategies to promote preconception health.
Conclusion
The evidence presented in this paper underscores the profound impact of alcohol consumption on fertility and preconception health. From disrupting the biochemical balance crucial for reproduction to its correlation with fertility issues, miscarriage rates, and fetal health complications, alcohol has been shown to negatively affect numerous aspects of reproductive health. Indirect effects, such as psychological and lifestyle factors associated with alcohol use, further exacerbate these impacts. In essence, the research clearly articulates the myriad ways in which alcohol consumption can be detrimental to those attempting to conceive and their potential offspring.
Research Gaps and Future Directions in Studying Alcohol's Impact on Fertility
Future research should continue to investigate these effects, especially in areas where there are still gaps in knowledge. For instance, more studies are needed to determine the exact mechanisms through which alcohol affects reproductive cells and hormones. Additionally, research should explore the impact of different patterns of alcohol consumption (such as binge drinking versus regular moderate drinking) on fertility and preconception health. Furthermore, it would be beneficial to examine the effectiveness of various strategies for reducing alcohol consumption among individuals trying to conceive.
Implications for Public Health Policy and Interventions
The implications for public health policy and interventions are significant. The evidence presented in this paper indicates a pressing need for comprehensive strategies to address the impact of alcohol on fertility and preconception health. These strategies should include public education campaigns to raise awareness about the risks associated with alcohol consumption, guidelines for healthcare professionals to provide consistent advice to patients, and policies to regulate alcohol advertising and availability.
In conclusion, the harmful effects of alcohol on fertility and preconception health are substantial and multifaceted. As such, it is crucial that individuals planning to conceive, healthcare professionals, and policymakers are aware of these risks. With a combined effort, it is possible to reduce these risks and contribute to healthier pregnancies and healthier future generations.
References
- Andersen, A. M. N., Andersen, P. K., Olsen, J., Grønbaek, M., & Strandberg-Larsen, K. (2012). Moderate alcohol intake during pregnancy and risk of fetal death. International Journal of Epidemiology, 41(2), 405-413.
- Bailey, B. A., & Sokol, R. J. (2011). Prenatal alcohol exposure and miscarriage, stillbirth, preterm delivery, and sudden infant death syndrome. Alcohol Research & Health, 34(1), 86.
- Bolúmar, F., Olsen, J., Rebagliato, M., & Sáez-Lloret, I. (1997). Caffeine intake and delayed conception: a European multicenter study on infertility and subfecundity. American Journal of Epidemiology, 145(4), 324-334.
- Centers for Disease Control and Prevention (CDC). (2020). Alcohol and Public Health. CDC. https://www.cdc.gov/ncbddd/fasd/alcohol-use.html
- Cook, R. L., & Clark, D. B. (2005). Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sexually transmitted diseases, 32(3), 156-164.
- Eggert, J., Theobald, H., & Engfeldt, P. (2004). Effects of alcohol consumption on female fertility during an 18-year period. Fertility and sterility, 81(2), 379-383.
- Hakonsen, L. B., Ernst, A., & Ramlau-Hansen, C. H. (2016). Maternal cigarette smoking during pregnancy and reproductive health in children: a review of epidemiological studies. Asian journal of andrology, 18(1), 39.
- Kasai, S., Shimizu, S., Tateno, H., Hoshi, K., & Yanagimachi, R. (2006). Effects of alcohol on sperm motility and fertilizing capacity in mice. Alcohol and Alcoholism, 41(4), 390-396.
- La Vignera, S., Condorelli, R. A., Balercia, G., Vicari, E., & Calogero, A. E. (2013). Does alcohol have any effect on male reproductive function? A review of literature. Asian journal of andrology, 15(2), 221.
- Louis, G. M. B., Lum, K. J., Sundaram, R., Chen, Z., Kim, S., Lynch, C. D., ... & Pyper, C. (2011). Stress reduces conception probabilities across the fertile window: evidence in support of relaxation. Fertility and sterility, 95(7), 2184-2189.
- May, P. A., Baete, A., Russo, J., Elliott, A. J., Blankenship, J., Kalberg, W. O., ... & Hoyme, H. E. (2014). Prevalence and characteristics of fetal alcohol spectrum disorders. Pediatrics, 134(5), 855-866.
- Mendelson, J. H., & Mello, N. K. (1988). Chronic alcohol effects on anterior pituitary and ovarian hormones in healthy women. Journal of Pharmacology and Experimental Therapeutics, 245(2), 407-412.
- National Institute for Health and Care Excellence (NICE). (2010). Pregnancy and complex social factors: A model for service provision for pregnant women with complex social factors. NICE. https://www.nice.org.uk/guidance/cg110
- National Health and Medical Research Council (NHMRC). (2020). Australian guidelines to reduce health risks from drinking alcohol. NHMRC. https://www.nhmrc.gov.au/health-advice/alcohol
- Patra, J., Bakker, R., Irving, H., Jaddoe, V. W., Malini, S., & Rehm, J. (2011). Dose–response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)—a systematic review and meta‐analyses. BJOG: An International Journal of Obstetrics & Gynaecology, 118(12), 1411-1421.
- Rasch, V. (2003). Cigarette, alcohol, and caffeine consumption: risk factors for spontaneous abortion. Acta obstetricia et gynecologica Scandinavica, 82(2), 182-188.
- Rehm, J., Room, R., Graham, K., Monteiro, M., Gmel, G., & Sempos, C. T. (2003). The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction, 98(9), 1209-1228.
- Windham, G. C., Von Behren, J., Fenster, L., Schaefer, C., & Swan, S. H. (1997). Moderate maternal alcohol consumption and risk of spontaneous abortion. Epidemiology, 8(5), 509-514.
- Zenzes, M. T., Puy, L. A., Bielecki, R., & Reed, T. E. (1997). Detection of benzo [a] pyrene diol epoxide-DNA adducts in embryos from smoking couples: evidence for transmission by spermatozoa. Molecular human reproduction, 3(2), 125-132.
- Emanuele, M. A., & Emanuele, N. (2001). Alcohol's effects on male reproduction. Alcohol Health & Research World, 25(4), 282.
- Hankin, J. R. (2002). Fetal alcohol syndrome prevention research. Alcohol Research & Health, 26(1), 58-65.
- Mikkelsen, E. M., Riis, A. H., Wise, L. A., Hatch, E. E., Rothman, K. J., & Sørensen, H. T. (2016). Alcohol consumption and fecundability: prospective Danish cohort study. Bmj, 354.
- Nulman, I., Rovet, J., Kennedy, D., Wasson, C., Gladstone, J., Fried, S., & Koren, G. (2004). Binge alcohol consumption by non-alcohol-dependent women during pregnancy affects child behavior, but not general intellectual functioning; a prospective controlled study. Archives of Women's Mental Health, 7(3), 173-181.
- Pfinder, M., Kunst, A. E., Feldmann, R., van Eijsden, M., & Vrijkotte, T. G. (2013). Preterm birth and small for gestational age in relation to alcohol consumption during pregnancy: stronger associations among vulnerable women? Results from two large Western-European studies. BMC pregnancy and childbirth, 13(1), 1-11.
- Viljoen, D. L., Gossage, J. P., Brooke, L., Adnams, C. M., Jones, K. L., Robinson, L. K., ... & May, P. A. (2005). Fetal alcohol syndrome epidemiology in a South African community: a second study of a very high prevalence area. Journal of studies on alcohol, 66(5), 593-604.