Discover the surprising benefits of Clomiphene Citrate for men, from boosting testosterone levels to increasing fertility.
Clomiphene citrate, commonly known as Clomid, is a medication that has long been used in women to induce ovulation. However, in recent years, there has been growing interest in its potential benefits for men’s health as well. This article aims to explore the various aspects of Clomiphene citrate use in men, from its mechanism of action to its potential benefits and risks.
Understanding Clomiphene Citrate
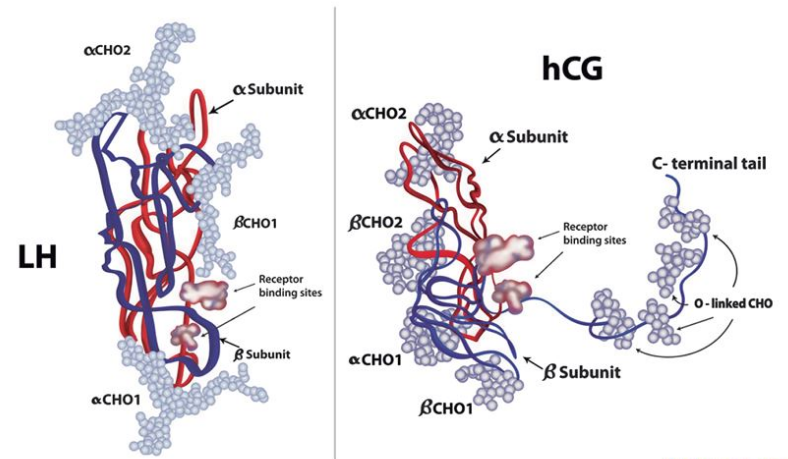
Before delving into the specifics, it’s important to understand what Clomiphene citrate is and how it works. Clomiphene citrate is a selective estrogen receptor modulator (SERM), meaning it has both estrogenic and anti-estrogenic effects, depending on the target tissue. It works by blocking the action of estrogen in certain tissues, including the hypothalamus, which leads to an increase in the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH).

Clomiphene citrate is commonly used in the treatment of female infertility, particularly in cases where ovulation induction is necessary. It is often prescribed to women who have irregular menstrual cycles or who do not ovulate regularly. By blocking estrogen receptors in the hypothalamus, Clomiphene citrate helps to “trick” the body into thinking that estrogen levels are low, leading to increased production of FSH and LH, which are essential for ovulation.
What is Clomiphene Citrate?
Clomiphene citrate is a white, crystalline powder that is orally administered. It is most commonly prescribed under the brand name Clomid and is available in various dosages. While it has primarily been used in women, it has also shown promise in men with certain health conditions.
In men, Clomiphene citrate is sometimes prescribed off-label to treat hypogonadism, a condition characterized by low testosterone levels. By stimulating the release of GnRH from the hypothalamus, Clomiphene citrate can help increase the production of FSH and LH, which in turn stimulates the testes to produce more testosterone. This approach can be beneficial for men looking to boost their testosterone levels without resorting to testosterone replacement therapy.
How Does Clomiphene Citrate Work?
The exact mechanism of action of Clomiphene citrate in men is not fully understood. However, it is believed to work by stimulating the release of gonadotropin-releasing hormone (GnRH) from the hypothalamus, which in turn stimulates the production and release of FSH and LH from the pituitary gland. This cascade of hormonal events ultimately leads to an increase in testosterone production.
It is important to note that Clomiphene citrate should only be used under the supervision of a healthcare provider, as improper use can lead to potential side effects and complications. Monitoring hormone levels and adjusting dosage as needed are crucial aspects of using Clomiphene citrate effectively and safely.
The Role of Clomiphene Citrate in Men’s Health
When it comes to men’s health, Clomiphene citrate has shown promise in two particular areas: testosterone levels and male fertility.
Clomiphene citrate, commonly known by its brand name Clomid, is a medication that has gained attention for its potential benefits in addressing hormonal imbalances in men. While traditionally used in women to stimulate ovulation, its off-label use in men has sparked interest in the medical community for its effects on testosterone levels and male fertility.
Clomiphene Citrate and Testosterone Levels
Low testosterone levels, or hypogonadism, can have a significant impact on a man’s overall health and well-being. Clomiphene citrate has been found to increase testosterone levels in men with hypogonadism, potentially alleviating symptoms such as fatigue, reduced libido, and erectile dysfunction. By acting as a selective estrogen receptor modulator (SERM), Clomiphene citrate stimulates the release of gonadotropins, which in turn signal the testes to produce more testosterone. This mechanism of action sets it apart from exogenous testosterone therapy, as it helps the body’s natural hormone production system.
It is important to highlight that while Clomiphene citrate can be effective in boosting testosterone levels, its use should be approached with caution. Regular monitoring of hormone levels and potential side effects is crucial to ensure its safe and appropriate use.
Impact on Male Fertility
Clomiphene citrate has also shown promise in improving male fertility. In men with suboptimal sperm parameters, Clomiphene citrate can increase sperm count, motility, and morphology. By stimulating the release of follicle-stimulating hormone (FSH) from the pituitary gland, Clomiphene citrate supports the maturation of sperm cells in the testes. This can be particularly beneficial for men seeking to enhance their fertility potential.
However, it is essential for individuals considering Clomiphene citrate for male fertility enhancement to consult with a reproductive specialist. The dosage and duration of treatment can vary based on specific sperm analysis results and underlying causes of infertility. Close monitoring and personalized care are key to maximizing the benefits of Clomiphene citrate in this context.
Potential Benefits of Clomiphene Citrate for Men
Beyond its impact on testosterone levels and male fertility, Clomiphene citrate has the potential for further benefits in men’s health.
Clomiphene citrate, commonly known as Clomid, is a medication typically used in the treatment of female infertility. However, its off-label use in men has garnered attention for its potential benefits beyond fertility.
Enhancing Physical Performance
There is emerging evidence suggesting that Clomiphene citrate may have positive effects on physical performance. Studies have shown that Clomiphene citrate can increase muscle strength, stamina, and overall athletic performance. These effects are thought to be due to the increase in testosterone levels and improved hormone balance. However, further research is needed to fully understand the extent and mechanisms behind these potential benefits.
In addition to its effects on muscle strength and athletic performance, Clomiphene citrate may also play a role in body composition. Some studies have indicated that it could lead to a reduction in body fat percentage and an increase in lean muscle mass, further contributing to improved physical performance and overall health.
Improving Sexual Health
Sexual health is an essential aspect of overall well-being, and Clomiphene citrate has shown promise in this area as well. Men with low testosterone levels often experience reduced libido and sexual dysfunction. By boosting testosterone production and restoring hormonal balance, Clomiphene citrate may help improve sexual desire, function, and satisfaction. However, it is important to consult with a healthcare professional to assess individual suitability and potential risks.
Furthermore, the potential benefits of Clomiphene citrate on sexual health extend beyond just libido and function. Some studies suggest that it may also have a positive impact on sperm quality, which can be crucial for men dealing with infertility issues. By improving both testosterone levels and sperm parameters, Clomiphene citrate offers a comprehensive approach to addressing male reproductive health.
Possible Side Effects and Risks
While Clomiphene citrate can offer potential benefits, it is essential to consider the possible side effects and risks associated with its use. Understanding the nuances of how this medication may affect your body is crucial for making informed decisions about your health and well-being.
It is important to note that individual responses to Clomiphene citrate can vary, and not everyone will experience the same side effects or risks. Factors such as dosage, duration of use, and underlying health conditions can all play a role in how a person may react to this medication.
Common Side Effects of Clomiphene Citrate
Some of the common side effects of Clomiphene citrate in men include hot flashes, mood swings, fatigue, headaches, and nausea. These side effects are usually mild and temporary, but it is crucial to discuss any concerns with a healthcare professional. Additionally, it is essential to be aware of any potential allergic reactions to the medication, such as rash, itching, swelling, or difficulty breathing, and seek immediate medical attention if any of these symptoms occur.
While the side effects mentioned are commonly reported, it is important to remember that not everyone will experience them to the same degree. Some individuals may have a higher tolerance for the medication, while others may be more sensitive to its effects. Monitoring your body’s response and communicating openly with your healthcare provider are key steps in managing any side effects that may arise.
Understanding the Risks and Precautions
As with any medication, Clomiphene citrate carries certain risks and precautions. It should not be used in men with liver disease, certain types of cancer, or a history of blood clotting disorders. It is important to undergo regular monitoring while on Clomiphene citrate to ensure its safe and effective use. Additionally, discussing any potential drug interactions with your healthcare provider is crucial, as certain medications or supplements may impact the effectiveness of Clomiphene citrate or increase the risk of adverse effects.
Furthermore, it is essential to consider the long-term implications of using Clomiphene citrate, especially in relation to fertility and hormonal balance. While the medication may offer benefits in certain cases, it is important to weigh these potential advantages against the risks and make an informed decision based on your individual health needs and goals.
The Medical Perspective on Clomiphene Citrate Use in Men
Clomiphene citrate, commonly known by its brand name Clomid, has garnered attention for its potential benefits in various aspects of men’s health. From addressing hypogonadism to aiding in male fertility and managing hormonal imbalances, this medication has shown promise in improving the well-being of men. However, the decision to prescribe Clomiphene citrate for specific medical conditions should always be made in consultation with healthcare professionals who can provide personalized guidance.
When considering the use of Clomiphene citrate in men, it is essential to understand the underlying reasons for its prescription. For individuals with hypogonadism, a condition characterized by low testosterone levels, Clomiphene citrate may help stimulate the production of this vital hormone. Similarly, in cases of male infertility where hormonal imbalances play a role, this medication could be part of a comprehensive treatment plan aimed at enhancing fertility.
When is Clomiphene Citrate Prescribed for Men?
Clomiphene citrate may be prescribed for men with hypogonadism, infertility, or certain hormonal imbalances. However, it is crucial to consult with a healthcare professional for a thorough evaluation and appropriate guidance regarding Clomiphene citrate use.
The Ongoing Research on Clomiphene Citrate
Research on Clomiphene citrate in men is still ongoing, with studies exploring its potential benefits and optimal usage guidelines. As more evidence emerges, our understanding of this medication’s role in men’s health will continue to evolve.
As researchers delve deeper into the effects of Clomiphene citrate on men’s health, they are uncovering new insights into its mechanisms of action and potential applications beyond the current scope of use. By elucidating the intricate ways in which this medication interacts with the male physiology, scientists aim to refine treatment protocols and maximize the benefits for patients.
Moreover, the exploration of Clomiphene citrate’s impact on male physical performance and sexual health represents a burgeoning area of interest within the medical community. Understanding how this medication influences not just hormonal levels but also overall well-being and quality of life is crucial for optimizing its therapeutic potential.