Discover how HCG can benefit men’s health and well-being.
The Benefits of HCG for Men: What You Need to Know
Human Chorionic Gonadotropin, commonly known as HCG, has gained popularity as a hormone therapy primarily used by women during pregnancy. However, what many people may not realize is that HCG also offers several benefits for men. In this article, we will explore the different aspects of HCG and its potential advantages for men’s health.
Understanding HCG: A Brief Overview
Before delving into the benefits of HCG for men, let’s first understand what HCG is and its role in the human body.
Human Chorionic Gonadotropin (HCG) is a fascinating hormone that holds a crucial place in the intricate workings of the human body. While its most well-known association is with pregnancy, where it is produced by the placenta to support the development of the fetus, HCG’s influence extends beyond the realm of reproduction.
What is HCG?
HCG is a hormone that is naturally produced in the body. It stands for Human Chorionic Gonadotropin and is primarily associated with pregnancy. It is produced by the placenta to support the growing fetus.
Interestingly, HCG is not only produced during pregnancy but also by certain tumors, making it a valuable marker in cancer diagnostics. Its presence in the body can indicate various medical conditions, highlighting the diverse roles this hormone plays in our health.
The Role of HCG in the Human Body
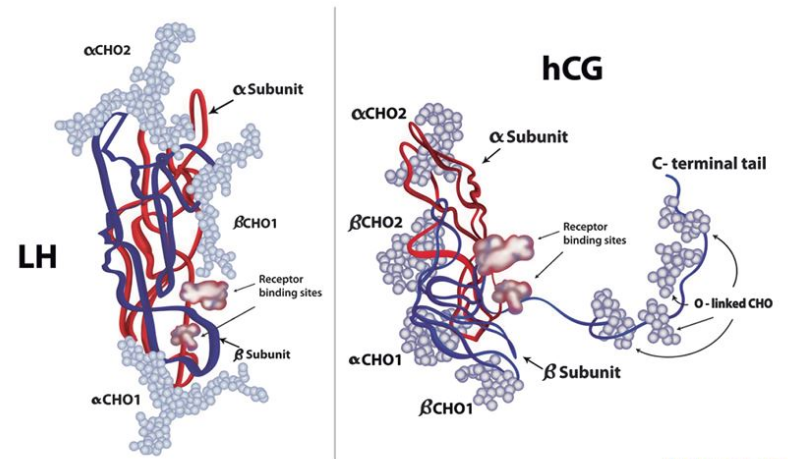
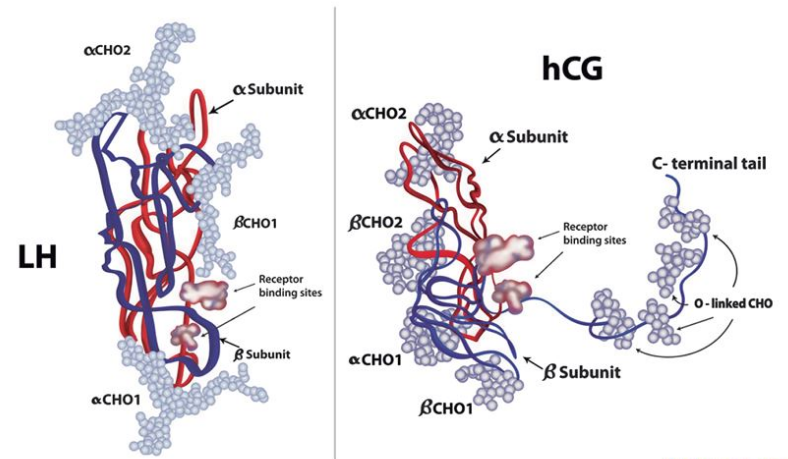
In addition to its role in pregnancy, HCG plays a significant role in regulating hormones and supporting various physiological processes in both men and women. For men, HCG is particularly crucial in maintaining adequate testosterone levels and promoting fertility.
Moreover, HCG has been utilized in various medical treatments beyond its reproductive functions. From aiding in weight loss to potentially improving testosterone production in men with hypogonadism, the versatility of HCG showcases the complexity of its actions within the human body.
The Importance of HCG for Men
Now that we have a basic understanding of HCG, let’s explore why it is essential for men’s health.
Human Chorionic Gonadotropin (HCG) is a hormone that plays a crucial role in male reproductive health. Beyond its well-known association with pregnancy, HCG also serves as a key player in supporting male fertility and hormonal balance.
HCG and Male Fertility
Male fertility depends on the production of healthy sperm. HCG stimulates the production of testosterone, which, in turn, increases sperm production. The administration of HCG can be beneficial for men experiencing fertility issues or those looking to enhance their fertility potential.
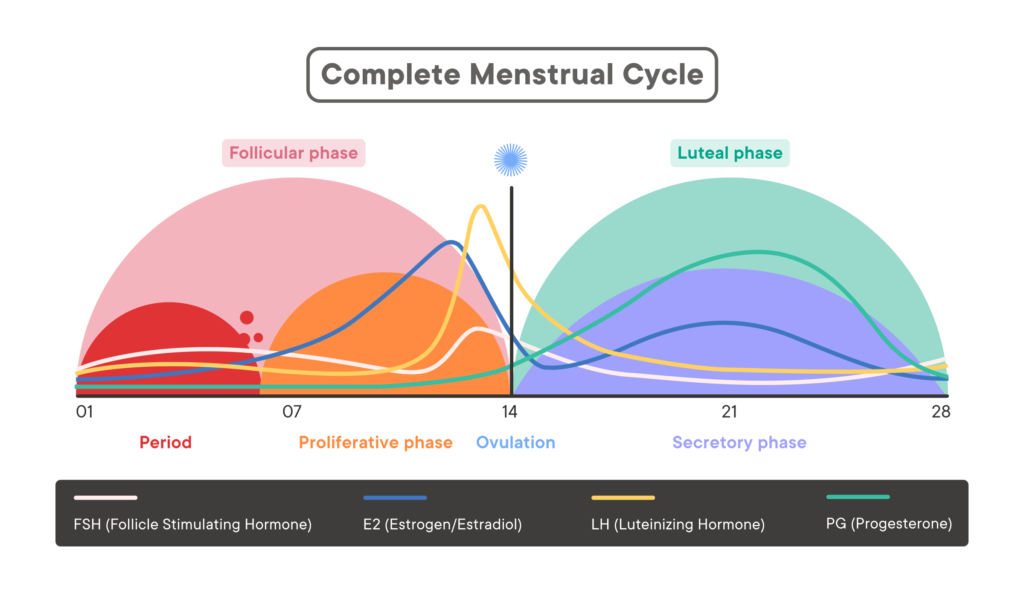
Furthermore, HCG not only aids in sperm production but also helps in maintaining the health and functionality of the testes. By mimicking the action of luteinizing hormone (LH), HCG supports the testes in producing testosterone and other androgens necessary for sperm maturation and overall reproductive health.
HCG’s Impact on Testosterone Levels
Testosterone is a vital hormone for men as it influences various aspects of their overall well-being. HCG promotes the production of testosterone, which is essential for maintaining muscle mass, bone density, and overall energy levels. Adequate testosterone levels also support libido and sexual function.

Moreover, HCG therapy has shown promising results in men with hypogonadism, a condition characterized by low testosterone levels. By stimulating the testes to produce more testosterone, HCG can help alleviate symptoms associated with low T, such as fatigue, decreased muscle mass, and mood disturbances.
Potential Health Benefits of HCG for Men
In addition to its role in fertility and testosterone production, HCG may offer several other potential health benefits for men.
Human Chorionic Gonadotropin (HCG) has gained attention for its potential to contribute to men’s health beyond its well-known roles. While primarily recognized for its involvement in fertility and testosterone production, emerging research suggests a broader spectrum of benefits that HCG may offer.
Weight Loss and Metabolism
Research suggests that HCG may aid in weight loss by suppressing appetite and increasing metabolism. This can be particularly beneficial for men who are struggling to shed excess pounds and improve their body composition.
Furthermore, HCG’s influence on metabolism goes beyond mere weight loss. By stimulating the body’s metabolic processes, HCG may assist in maintaining a healthy weight in the long term, supporting overall well-being and vitality.
Muscle Growth and Recovery
As mentioned earlier, HCG promotes testosterone production, which is essential for muscle growth and recovery. By increasing testosterone levels, HCG may help men achieve better results from their workouts, enhance muscle strength, and facilitate faster recovery after intense physical activity.
Moreover, the potential synergy between HCG and exercise cannot be overlooked. When combined with a structured workout regimen, HCG’s ability to support muscle growth and recovery may lead to more efficient and effective fitness outcomes for men seeking to optimize their physical performance.
Mood and Energy Levels
HCG’s impact on testosterone levels can also influence mood and energy levels. Low testosterone levels can lead to fatigue, depression, and reduced motivation. By maintaining optimal testosterone levels, HCG may help improve overall mood and energy levels.
Furthermore, the interplay between hormonal balance and mental well-being underscores the importance of considering holistic approaches to men’s health. By addressing both physical and emotional aspects, HCG’s potential to enhance mood and energy levels may contribute to a more comprehensive sense of wellness and vitality.
Risks and Side Effects of HCG Use in Men
While HCG offers several potential benefits, it is crucial to be aware of the possible risks and side effects associated with its use in men.
Human Chorionic Gonadotropin (HCG) is a hormone that is naturally produced in the body, but when used exogenously, it can have various effects on male physiology. One of the key considerations when using HCG in men is its impact on the endocrine system, particularly the delicate balance of hormones that regulate reproductive and sexual function.
Possible Short-Term Side Effects
Some men may experience side effects such as headache, water retention, breast enlargement, and changes in mood. These side effects are typically temporary and subside once the HCG treatment is discontinued.
It is essential for individuals considering HCG therapy to be aware of these potential short-term side effects and to consult with a healthcare provider if they experience any concerning symptoms. Monitoring and adjusting the dosage of HCG can help mitigate these side effects and ensure a more comfortable treatment experience.
Long-Term Risks and Considerations
Long-term use of HCG may have certain risks, including the potential suppression of natural testosterone production. It is important to work closely with a healthcare professional who specializes in hormone therapy to monitor testosterone levels and ensure optimal safety and efficacy.
Furthermore, prolonged use of HCG in men may also impact fertility by disrupting the body’s natural feedback mechanisms that control sperm production. This is a crucial consideration for individuals who are planning to maintain or enhance their fertility while undergoing HCG therapy.
How to Use HCG: Guidelines and Recommendations
If you are considering HCG therapy, it is essential to follow the appropriate guidelines and recommendations.
Human Chorionic Gonadotropin (HCG) is a hormone that plays a crucial role in various bodily functions, including fertility and testosterone production. When used therapeutically, HCG can offer a range of benefits for men’s health.
Dosage and Administration
HCG can be administered through injections or oral supplements. The dosage and administration method may vary based on individual needs and the advice of a healthcare professional. It is crucial to follow the prescribed dosage and adhere to the recommended administration schedule.
Typically, HCG injections are given intramuscularly, with the dosage tailored to the individual’s specific requirements. Oral HCG supplements are also available, but their efficacy and absorption rates may differ from injectable forms.
When to Seek Medical Advice
It is crucial to seek medical advice before starting HCG therapy. A healthcare professional can evaluate your specific needs, assess any underlying health conditions, and determine if HCG therapy is suitable for you. They can provide personalized guidance and monitoring to ensure optimal results and minimize potential risks.
Furthermore, regular monitoring of hormone levels, including testosterone and estradiol, is essential during HCG therapy to ensure that the treatment is effective and well-tolerated. Adjustments to the dosage or administration method may be necessary based on these hormone levels.
In conclusion, HCG offers several potential benefits for men’s health. From promoting fertility to enhancing testosterone levels and supporting overall well-being, HCG therapy may be beneficial for men experiencing certain health concerns or looking to optimize their health. However, it is crucial to seek medical advice and closely monitor testosterone levels to ensure safe and effective use of HCG.